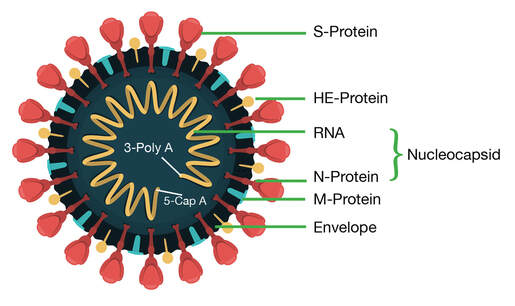
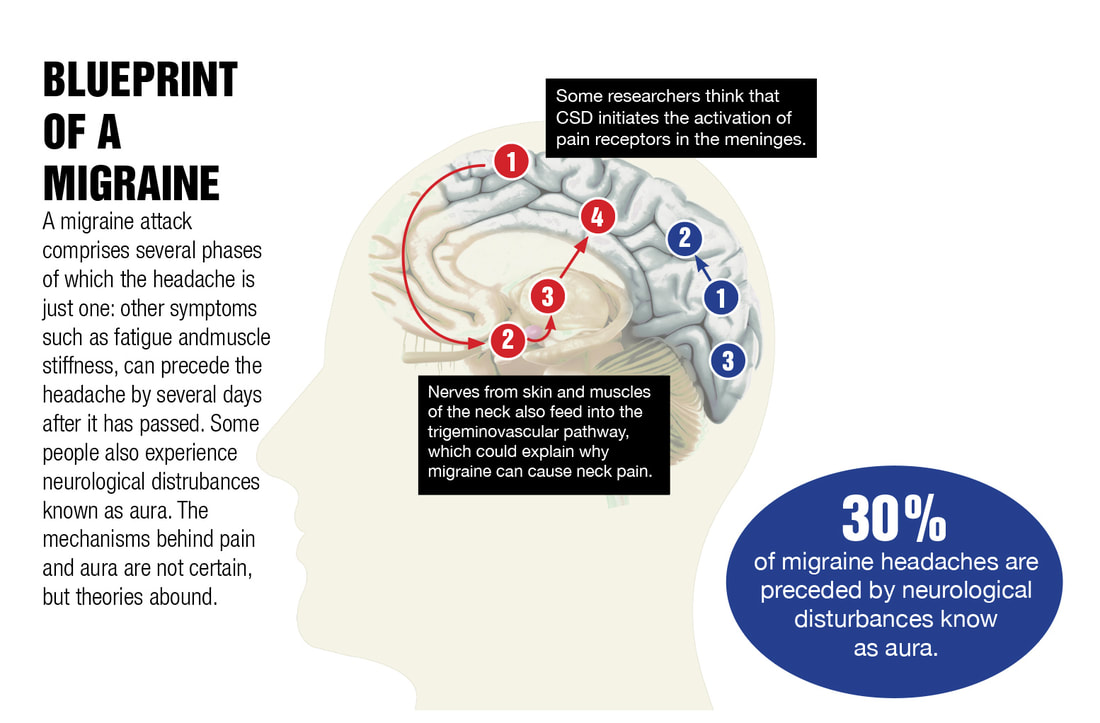
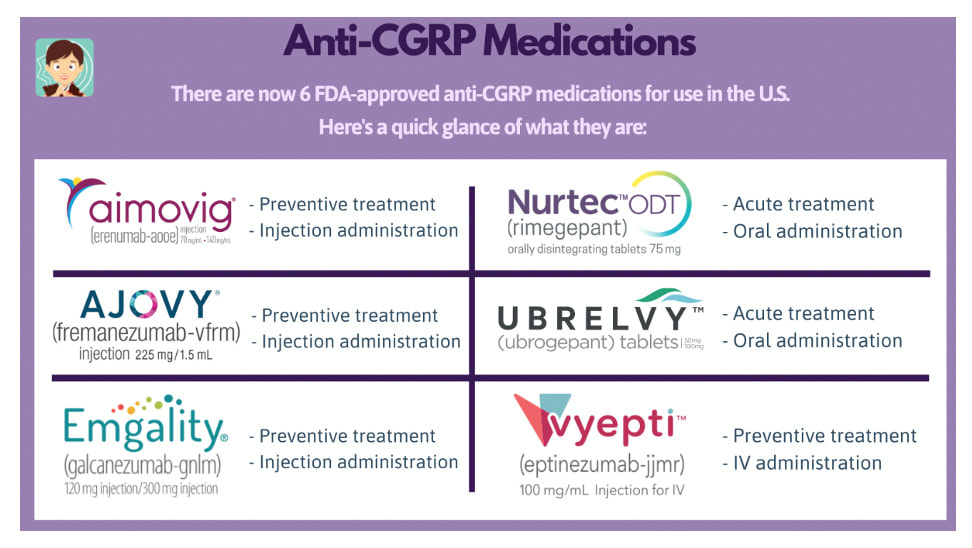
And we are also seeing a tremendous rise of long COVID symptomatology after injections of the COVID vaccines. This is due to the inherent nature of how these experimental products are designed to work. We understand now that most of the severe outcomes from SARS COV 2 infections and the mechanisms behind long COVID are not necessarily a result of the virus itself but are due to spike protein component. Spike protein, depicted on the outside of the virus, is what allows the virus to attach to a binding domain called the ACE 2 receptor that allows entry of the virus into the cell for replications. We know that spike protein on its own has been found to be toxic to both the body and brain. Each of the COVID vaccines use a mechanism that sends a genetic code to every cell in your body to launch the production of trillions of spike proteins. Spike protein has been shown to promote inflammatory responses, induce thrombogenesis, alter the innate and adaptive immunity, and can disrupt the blood-brain barrier (BBB), all of which are mechanisms which could explain related symptoms, ranging from dizziness, headache, and loss of concentration to microclots, encephalitis, etc as noted in a recent study. Neurological symptoms are experienced by 30 to 80 percent of patients with Long COVID. And while new cases of SARS CoV 2 and its Omicron variant are occurring with less frequency and severity, we are still seeing an alarming rise of long COVID incidence. Headache in long COVID. Headache during the acute phase of COVID-19 is shared and reported between 34 and 75% of patients.1 However, nearly one-third of patients experienced long-lasting symptoms; clinicians note that it is difficult to treat headaches with various presentations as this suggests equally distinct pathophysiological mechanisms. And about half of these patients have no previous history of headache. Why is headache so common? During the acute infection, headache may be caused by circulating inflammatory mediators activating the trigeminovascular system at the meninges. The dura trigeminal ganglion neurons lead to the release of neuropeptides, including calcitonin gene-related peptide (CGRP) and substance P from their nerve terminals, leading to vasodilation and plasma extravasation. The trigeminal nerve mediates pain sensation from cranial structures in the anterior two-third of the head and plays a crucial role for the headache phase.2 What is CGRP and what are the CGRP inhibitors? CGRP or calcitonin gene-related peptide is a 37-amino acid sensory neurotransmitter that is widely distributed throughout both the central and the peripheral nervous system. This CGRP protein is released by pulmonary nerve endings during viral infection and participates in regulating the immunoinflammatory response.3 Elevated circulating CGRP levels may cause headache in predisposed individuals in the context of acute COVID-19. CGRP plays a key role in several mechanisms of migraine pathology and pain perception, including vasodilation, neurogenic inflammation, mast cell degranulation, sensory signaling activation and peripheral sensitization.4 In 2018, the FDA approved three new migraine medications -- erenumab (Aimovig), fremanezumab (Ajovy), and galcanezumab (Emgality) -- which are in a class of drugs called monoclonal antibodies. These "targeted" therapies seek out and interfere with CGRP. For that reason, the drugs are also known as CGRP antagonists or CGRP inhibitors. They can block and neutralize CGRP for weeks at a time and typically are given as a monthly injection. Some recent research has shown CGRP inhibitors also could be used to down-regulate pro-inflammatory macrophages. About macrophages and CGRP… Macrophages are immune cells that release cytokines, small proteins that signal the immune system to do its job – but the overproduction of these proteins in the presence of an infection, for example, can result in a cytokine storm and severe inflammatory reaction. CGRP is released from peripheral nerves and plays a role in neuropathic pain. Some recent research has shown CGRP inhibitors could be used to down-regulate pro-inflammatory macrophages. In the case of a long-hauler protocol, one element is shifting pro-inflammatory to anti-inflammatory cytokines of macrophages using H1 and H2 blockers and or various supplements Learn more at: https://www.suzannegazdamd.com/blog/what-if-there-was-another-way-to-treat-neuropathic-pain Mechanisms Underlying Headache in Long COVID
Based on the work of Dr. Bruce Patterson and other clinicians, we know that high levels of proinflammatory cytokines are present in long Haulers who had even a mild SARS COV 2 infection and in the post-vaccine injured.6 We also know now that spike protein can alter the integrity of and cross the BBB, which could trigger an extreme amount of neuroinflammation.7
In this recent publication it is thought that the activation of the trigeminovascular system is due to protein mimicry between CGRP receptors and antibodies against SARS-CoV-2 spike protein I have discussed before the study by Dr. Vorjdani et al that showed molecular mimicry with 28 out 55 human tissues to spike protein and other viral fragments of SARS-CoV-2. So, once again, we are seeing the downstream effects of molecular mimicry here with migraine and headache in long COVID. This mechanism may explain the higher frequency of headaches and why a persistent headache occurs in COVID-19 specifically rather than other viral systemic infections and as well why headache is such a common symptom in the vaccine injured. Circulating antibodies against spike protein continue to interact with the CGRP receptor which could limit the response to CGRP inhibitors.8
In long COVID, extensive fibrin amyloid microclots can persist, entrap other proteins, and may lead to the production of various autoantibodies that further induce inflammation pathways. Inflammatory pathways are also activated when the ACE2 receptor is dysregulated by spike protein. ACE2 is a vital element in a biochemical pathway that is critical to regulating processes such as blood pressure, wound healing, and inflammation, called the renin-angiotensin-aldosterone system (RAAS) pathway. When the SARS-CoV-2 virus/spike protein binds to ACE2, it prevents ACE2 from performing its normal function to regulate these functions including ANG II signaling. Angiotensin II (Ang II) is a protein that increases blood pressure and inflammation, increasing damage to blood vessel linings and various types of tissue injury. ACE 2 receptors are found on platelets, which are blood cells that help with clotting. And, they’re also found on the endothelium, which is the innermost lining of the blood vessels. By binding to the platelets and the endothelium, the virus/ spike protein sets off a clotting cascade, and as a result is vascular inflammation and risk of thrombosis ACE 2 blocking or inhibition can increase norepinephrine and serotonin action on vascular tone. Dysregulation of ACE 2 is implicated in stroke, cognitive decline, Alzheimer’s disease and Parkinson’s disease, and pain ACE 2 inhibitors in migraine.9 Unbalanced vasoconstriction, oxidative stress, and free radical formation upon downregulation and internalization of transmembrane ACE2 by the virus/spike protein binding may lead to a vasculopathy. A model of endothelial dysfunction in the trigeminovascular system has emerged in migraine research. Endothelial dysfunction induces an inflammatory response which results in oxidative stress and a hypercoagulable state marked by increased platelet reactivity, altered erythrocyte morphology and metabolism, and increased fibrinogen levels. What else may be contributing to long COVID neurological symptoms? Brainstem Dysfunction in Long Covid. One more potential cause of long-COVID could be the brainstem tropism of SARS-CoV-2 and the resulting persistent, low-grade brainstem dysfunction. The brainstem has a relatively high expression of ACE2 receptor compared with other brain regions. As posited by the study, these support the hypothesis that brainstem sensitivity fluctuates throughout the migraine cycle.10 Elevated Glutamate. Glutamate is the most abundant neurotransmitter in our brain and central nervous system (CNS). It is involved in virtually every major excitatory brain function Glutamate exerts its effects on brain excitability via the N-methyl-d-aspartate (NMDA), AMPA (alpha-amino-3-hydroxy-5-methyl-4-isoxazole-propionate), kainite, and metabotropic glutamate receptors. In this article the many mechanisms of how COVID 19 affects the brain are reviewed, noting that increased quinolinic acid results in higher glutamate and upregulation of NMDA receptors, possibly inducing altered learning and memory.11 Glutamate receptors have also been studied as a potential target for migraine treatment. One of them is called memantine; memantine is a moderate-affinity uncompetitive NMDA receptor antagonist that is approved in the U.S. for the treatment of Alzheimer’s disease. So, how do we conduct an appropriate evaluation in cases of long COVID-related headache? It is important for long hauler patients to have a full evaluation if presenting with severe and/or atypical headaches. Magnetic resonance imaging (MRI), complete lab workup, and in some instances, a lumbar puncture may be needed. In my practice’s evaluations, I also include a NeuroQuant done on a MRI with CoreTech software. Sometimes additional imaging is necessary, such as a MRA (magnetic resonance arteriogram) or MRV (magnetic resonance venogram); a lumbar puncture may be needed as well depending on individual needs. Serious life-threatening etiologies may underlie some of these presenting symptoms especially post vaccination, such as venous sinus thrombosis, vasculitis, encephalitis, intracranial bleed, pseudotumor cerebri, invasive sinusitis, uncontrolled blood pressure, and others. In this report, researchers present evidence that vaccine-induced thrombotic thrombocytopenia (VITT) without associated cerebral venous sinus thrombosis (CVST) or other thromboses and with severe headache as the heraldic symptom may precede VITT (“pre-VITT syndrome”). Additionally, a recent case report of MOGAD after the Johnson & Johnson vaccine was reported, with one patient presenting with severe headache following administration of the vaccine. MOGAD is most frequently associated with optic neuritis in adults and acute disseminated encephalomyelitis in children, which often encompasses longitudinally extensive transverse myelitis and brainstem encephalitis. An MR, lab and sometimes a lumbar puncture is needed to diagnose and assess. Perhaps most important, patients who are experiencing headache or other lingering symptoms of long COVID should consult a clinician with experience in treating this very complex syndrome. Talk to your physician for guidance or referral for specialized care and don’t hesitate to reach out to our offices if we can help. And be sure to catch up on our complete long COVID series of blogs for additional valuable information and more details: https://www.suzannegazdamd.com/blog---long-covid In hope and healing, Dr. Suzanne Gazda References: 1 Özkan E, Celebi Ö, Keskin Ö, Gursoy A and Gürsoy-Özdemir Y (2022) Is Persistent Post-COVID Headache Associated With Protein-Protein Interactions Between Antibodies Against Viral Spike Protein and CGRP Receptor?: A Case Report. Front. Pain Res. 3:858709. doi: 10.3389/fpain.2022.858709 2 Edvinsson, J.C.A., Viganò, A., Alekseeva, A. et al. The fifth cranial nerve in headaches. J Headache Pain 21, 65 (2020). https://doi.org/10.1186/s10194-020-01134-1 3 J.A. Membrilla, E. Caronna, J. Trigo-López, A. González-Martínez, A. Layos-Romero, P. Pozo-Rosich, Á. Guerrero-Peral, A.B. Gago-Veiga, A. Andrés-López, J. Díaz de Terán. Persistent headache after COVID-19: Pathophysioloy, clinic and treatment. Neurology Perspectives. Volume 1, Supplement 1, 2021. Pages S31-S36, ISSN 2667-0496. https://doi.org/10.1016/j.neurop.2021.10.003 4 Russell FA, King R, Smillie SJ, Kodji X, Brain SD. Calcitonin gene-related peptide: physiology and pathophysiology. Physiol Rev. 2014;94(4):1099-1142. doi:10.1152/physrev.00034.2013 5 Low, R. N., Low, R. J., & Akrami, A. (2020, November 12). A Cytokine-based model for the pathophysiology of Long COVID symptoms. https://doi.org/10.31219/osf.io/7gcnv 6 Patterson, Bruce K et al. “Immune-Based Prediction of COVID-19 Severity and Chronicity Decoded Using Machine Learning.” Frontiers in immunology vol. 12 700782. 28 Jun. 2021, doi:10.3389/fimmu.2021.700782 7 Rhea, E.M., Logsdon, A.F., Hansen, K.M. et al. The S1 protein of SARS-CoV-2 crosses the blood–brain barrier in mice. Nat Neurosci 24, 368–378 (2021). https://doi.org/10.1038/s41593-020-00771-8 8 Özkan E, Celebi Ö, Keskin Ö, Gursoy A and Gürsoy-Özdemir Y (2022) Is Persistent Post-COVID Headache Associated With Protein-Protein Interactions Between Antibodies Against Viral Spike Protein and CGRP Receptor?: A Case Report. Front. Pain Res. 3:858709. doi: 10.3389/fpain.2022.858709 9 Nandha R, Singh H. Renin angiotensin system: A novel target for migraine prophylaxis. Indian J Pharmacol. 2012;44(2):157-160. doi:10.4103/0253-7613.93840 10 Marciszewski KK, Meylakh N, Di Pietro F, et al. Changes in Brainstem Pain Modulation Circuitry Function over the Migraine Cycle. J Neurosci. 2018;38(49):10479-10488. doi:10.1523/JNEUROSCI.1088-18.2018 11 Boldrini M, Canoll PD, Klein RS. How COVID-19 Affects the Brain. JAMA Psychiatry. 2021;78(6):682–683. doi:10.1001/jamapsychiatry.2021.0500 For additional related subject matter reading, see: Memantine for headache https://www.uspharmacist.com/article/memantine-for-the-treatment-of-migraine Neuroinflammation https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5025335/ Headache pain https://thejournalofheadacheandpain.biomedcentral.com/articles/10.1186/s10194-021-01271-1 Cerebral thrombosis post COVID https://www.sciencedirect.com/science/article/pii/S2214751921000037 Delayed headache after COVID vaccine from thrombosis https://thejournalofheadacheandpain.biomedcentral.com/articles/10.1186/s10194-021-01324-5 Vaccine-induced thromobocytopenia https://www.nejm.org/doi/full/10.1056/NEJMc2112974 Vaccine induced Thrombocytopenia Immune complex disease after COVID https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-021-06655-x Large vessel vasculitis https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8784224/ COVID and benign intracranial hypertension (BIH) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7294953/ Case report BIH post vaccine https://www.medicalandresearch.com/assets/articles/documents/DOCUMENT_20220303161130.pdf Activation of the trigeminal system as a likely target of SARS-CoV-2 may contribute to anosmia in COVID-19 https://journals.sagepub.com/doi/full/10.1177/03331024211036665 A possible role of blood clotting in migraine https://www.frontiersin.org/articles/10.3389/fneur.2019.01262/full COVID vaccine and CNS inflammation https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8417681/ Persistent headache after COVID-19: Pathophysioloy, clinic and treatment https://www.sciencedirect.com/science/article/pii/S2667049621000685
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorSuzanne Gazda M.D. Neurologist Archives
January 2024
Categories |

 RSS Feed
RSS Feed