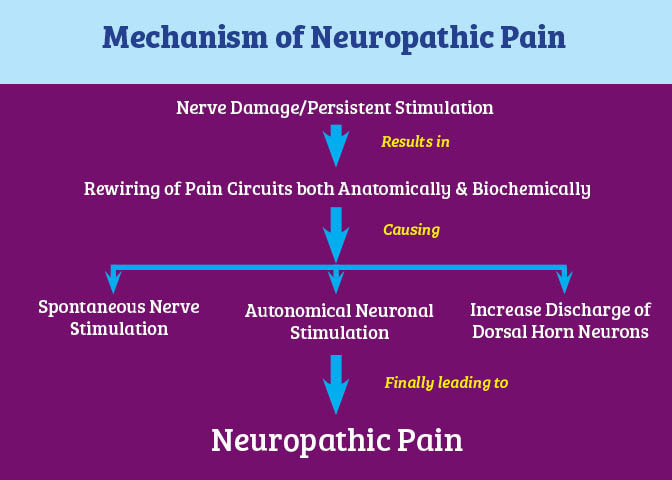
The severity and causes of neuropathy vary and can include diabetes and neurological or autoimmune disorders like lupus or Guillain-Barre syndrome. Unfortunately the single-most common denominator perhaps has been the lack of effective treatment -- there are just very few options available to physicians to provide symptomatic relief through medications or otherwise. And as we are already seeing every day with an increasing number of “long-hauler” post-COVID patients, there is commensurately an even greater need now to find more ways to resolve neuropathic pain associated with all of these conditions. But what if it was possible to employ a similar protocol used in migraine treatments that addresses this same type of underlying inflammation which we know is present in virtually every condition? And could the neuropathy also be improved? Let’s talk about CGRP inhibitors and macrophages. What do CGRP inhibitors and macrophages have to do with addressing neuropathic pain? First, CGRP or calcitonin gene-related peptide (CGRP) inhibitors are a relatively new class of medications designed to block the effect of CGRP, which is a small protein found in the sensory nerves that supply the head and the neck. CGRP is involved in pain transmission and in the case of migraine, for example, levels increase during an attack. 2 Macrophages are cells involved in the detection and destruction of bacteria and other harmful organisms. One of the major components of the inflammatory process, they can play an important role in eliminating diseased and damaged cells through their programmed cell death. As such, macrophages release cytokines, small proteins that signal the immune system to do its job – but the overproduction of these proteins in the presence of an infection, for example, can result in a cytokine storm and severe inflammatory reaction.3 Some recent research has shown CGRP inhibitors could be used to down-regulate pro-inflammatory macrophages. In the case of a long-hauler protocol, one element is shifting pro-inflammatory to anti-inflammatory cytokines or macrophages using H1 and H2 blockers. Steroids work the same way, as do non-steroidal anti-inflammatory drugs (NSAIDs) and gabapentin. Also, with intravenous immunoglobulin (IVIG), there are multiple mechanisms that can reduce inflammation in both the brain and system-wide.4 Scientists in Denmark studying patients with diabetes-related peripheral neuropathy (DPN) identified several significant findings that point to the role of inflammation in the resulting peripheral pain. Many factors are known to contribute to neuropathic pain in diabetes, including the release of the neuropeptide substance P (SP) and CGRP from sensory nerve terminals and inflammatory mediators (cytokines) from immune cells. The investigators found that “increased macrophages and increased CGRP-expressing and SP-expressing nerve fibers in the skin of patients with P-DPN may be consistent with a role of the immune system and neuropeptides in driving pain in DPN.”5
If inhibiting CGRP offers relief in these instances of diabetic neuropathic pain, could they then also provide relief in other applications? This is a fascinating study and one that does offer more hope to a spectrum of patients suffering with debilitating and ongoing symptoms. And we look forward to seeing additional research that can support the development of more therapies for all those who live with this type of chronic pain. In hope and healing, Dr. Suzanne Gazda For additional reading about IVIG, please see these and other related articles in our blog archives at: https://www.suzannegazdamd.com/blog/ivig-in-autoimmune-disease-therapies https://www.suzannegazdamd.com/blog/with-more-potential-uses-for-more-diseases-ivig-gains-enhanced-awareness-for-its-multimodal-properties References: 1 Cleveland Clinic, www.clevelandclinic.org 2 Mohanty D, Lippmann S. CGRP Inhibitors for Migraine. Innov Clin Neurosci. 2020;17(4-6):39-40. 3 Arango Duque G and Descoteaux A (2014) Macrophage cytokines: involvement in immunity and infectious diseases. Front. Immunol. 5:491. doi: 10.3389/fimmu.2014.00491 4 Saha C, Kothapalli P, Patil V, ManjunathaReddy GB, Kaveri SV, Bayry J. Intravenous immunoglobulin suppresses the polarization of both classically and alternatively activated macrophages. Hum Vaccin Immunother. 2020;16(2):233-239. doi:10.1080/21645515.2019.1602434 5 Sandra Sif Gylfadottir, Mustapha Itani, Alexander Gramm Kristensen, et al. Analysis of Macrophages and Peptidergic Fibers in the Skin of Patients With Painful Diabetic Polyneuropathy. Neurol Neuroimmunol Neuroinflamm Jan 2022, 9 (1) e1111; DOI: 10.1212/NXI.0000000000001111
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorDr. Suzanne Gazda, Integrative Neurology Archives
February 2024
Categories |

 RSS Feed
RSS Feed