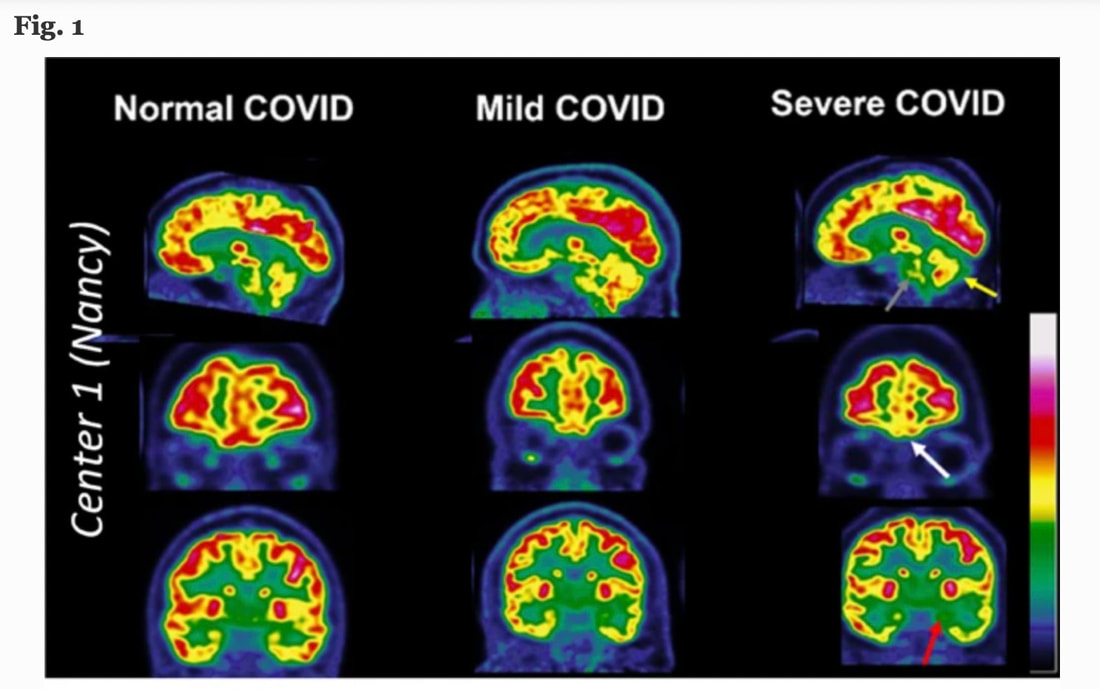
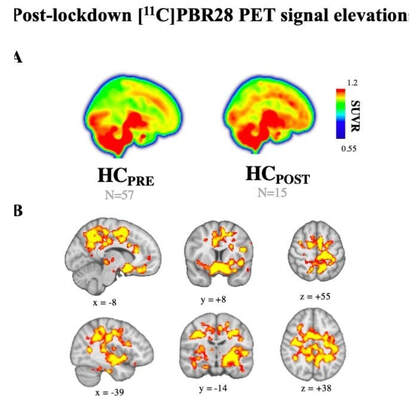
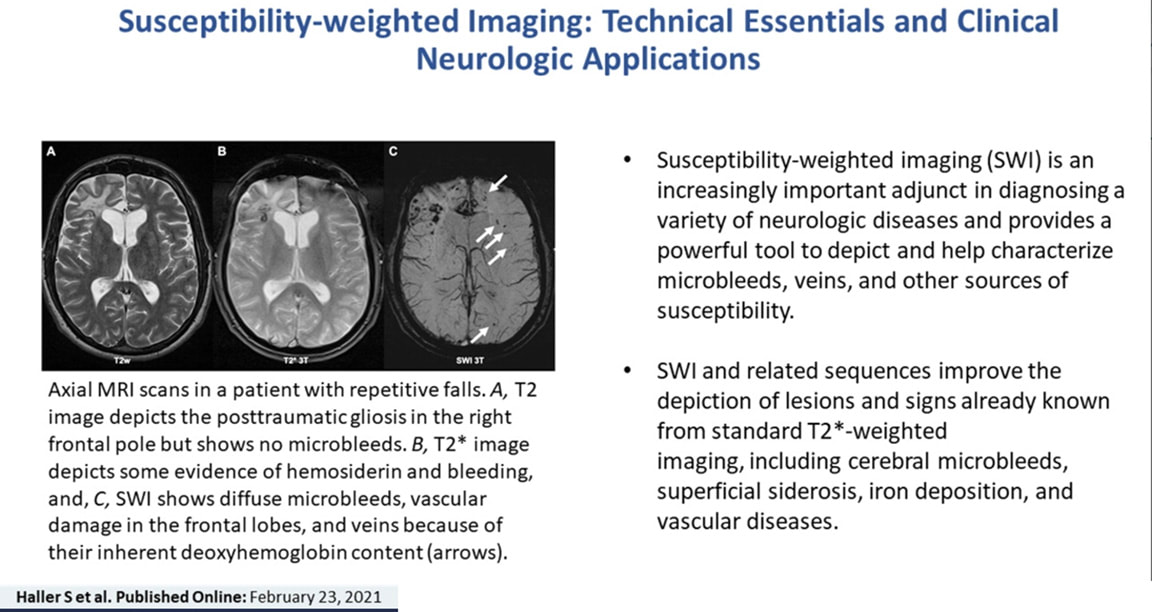
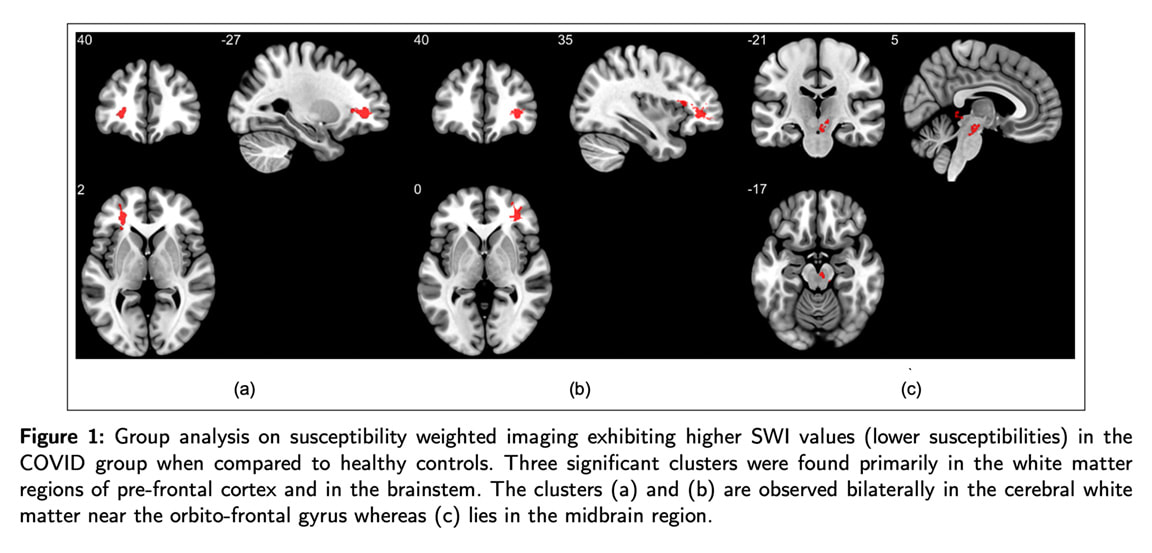
The study employed susceptibility-weighted imaging (SWI), which combines the phase and magnitude information from magnetic resonance imaging (MRI). As stated in the preprint abstract, “The three-dimensional high-resolution gradient echo (GRE) sequence used in the SWI modality enables it to utilize the phase data. When combined in a specific manner with these phase data the magnitude data yields SWI volumes.” Analyses of the results suggest an association of long COVID with prolonged effects on the brain and also indicates the viability of SWI modality for analysis of post-COVID symptoms…which ideally could provide another tool in the hands of clinicians who are treating multiple patients now suffering with this novel disorder. More about the study is discussed further down in this blog, so please keep reading to learn about it and other imaging technologies that could potentially offer additional critical insights. A closer look at the pandemic brain. Mild to severe psychological, behavioral, and cognitive sequelae in COVID-19 survivors have been reported. Thousands of vaccine injuries have also been reported to the CDC with recent data showing a total of 1,447,520 reports of adverse events following COVID-19 vaccines were submitted between Dec. 14, 2020, and Oct. 21, 2022, to the Vaccine Adverse Event Reporting System (VAERS). Current data indicates that up to 70 % of long COVID patients are experiencing signs of cognitive dysfunction. It is estimated that approximately one in five adults will develop long-term effects from COVID-19, according to the U.S. Centers for Disease Control and Prevention (CDC). But some studies have shown the numbers could be as high as 50%, a grave concern I have discussed in my previous blog: https://www.suzannegazdamd.com/blog---long-covid/do-we-have-a-new-form-of-alzheimers-disease-in-the-making I also have written about the tsunami of neurological injuries now upon us in the nearly three years since COVID was first identified. This considers the vast population affected by this pandemic which at this writing includes over 524 million people worldwide and the shocking rise in the number of those injured after the COVID vaccination. Therefore, quantitating the numbers of patients affected by the pandemic becomes almost impossible these days. Regardless of the data sets, long COVID is a global event affecting millions of patients…with no end in sight to the exponential rise in patients. Patients with neurological symptoms related to long COVID are struggling to find answers but many times are dismissed as “no objective data” can be found. So it’s imperative we identify additional means to better study the brain in order to identify the treatments so urgently needed in clinical practice. PET Scans. Multiple studies on COVID patients using positron emission tomography (PET) and computerized tomography (CT) imaging have consistently reported hypometabolism of fludeoxyglucose (FDG) in the frontal lobe of the brain. FDG is a radiopharmaceutical, specifically a radiotracer, used in PET imaging. After examining PET images of patients with suspected long COVID, a study published in the European Journal of Nuclear Medicine and Molecular Imaging identified hypometabolic patterns in nearly half of all patients. Each of the 143 patients was experiencing neurological symptoms at the time of the 18F-FDG PET scan, such as fatigue, pain, memory or cognitive complaints and insomnia. On average, the scans were conducted 10.9 months after the onset of these symptoms. Note: in clinical practice it is nearly impossible to get a PET scan, which can cost ~$8,000 out-of-pocket, covered by most insurance carriers Visual interpretation of brain hypometabolism related to neurological long COVID: a French multicentric experience. Springer, March 23, 2022 MRI finding in the UK Biobank Study. Research into the brain MRIs of individuals who recovered from COVID-19 cases has revealed that post COVID, the brain takes a huge hit. Based on the brain scans of more than 700 UK Biobank participants, researchers identified changes in the gray matter of individuals who had been infected with COVID, despite their illnesses being considered mild in nature. The UK Biobank is a large-scale, regularly updated biomedical database and research resource, containing in-depth genetic and health information from half a million UK participants; you can learn more about their programs at: https://www.ukbiobank.ac.uk/ For comparative purposes, the brain scans from individuals who had never acquired the virus—but had shared demographics such as age, gender, and COVID risk factors—were also incorporated in the study. Participants waited an average of 141 days between COVID diagnosis and their second brain MRI. They noted a reduction of gray matter thickness in the areas of the orbitofrontal cortex and parahippocampal gyrus, both of which impact memory processing and in the primary olfactory cortex. The COVID group also showed a loss of overall brain size and displayed signs of increased cognitive decline. Importantly, when the individuals who were hospitalized were excluded from the data, the findings remained consistent, signaling that even milder cases of COVID come with neurologic consequences. Also, observations made from the PET/MRI brain scans of individuals who have not been infected with COVID-19 prove that no one is immune to the effects of the pandemic. A study published in Brain, Behavior, and Immunity noted high levels of neuroinflammation were found in what they authors termed “the Pandemic Brain.” From Brain, Behavior, and Immunity Volume 102, May 2022, Pages 89-97 Susceptibility weighted imaging and long COVID. As we stated at the beginning of this article, data from a recent study showed that at six months post-COVID recovery, patients had brain MRI's with significantly higher susceptibility values in the frontal lobe and brain stem compared to healthy controls. These brain regions are linked with fatigue, insomnia, anxiety, depression, headaches, and cognitive problems. Susceptibility weighted imaging (SWI) is a relatively new MRI technique. It works by taking advantage of the different responses of certain materials – such as blood components, calcium, and iron – when they are exposed to a magnetic field. SWI is particularly useful for identifying and locating brain hemorrhages, vascular malformations, and tumors. Magnetic susceptibility denotes how much certain materials, such as blood, iron and calcium, will become magnetized in an applied magnetic field. It can be helpful in evaluating patients presenting with stroke or traumatic brain injury (TBI) where we look for evaluation of diffuse axonal injury that may result from a blunt force event (i.e. auto accident) and cause the brain to shift and rotate inside the skull. As such, SWI technique is useful in detecting several pathologies in white and gray matter and conditions such as microhemorrhages, cerebral microbleeds, vascular malformations, trauma, amyloid angiopathy associated with dementia and multiple sclerosis. Microhemorrhages associated with Alzheimer's disease may be an underestimated cause of progressive cognitive impairment in the elderly.
SWI Study Design. Researchers recruited a sample of patients (46 COVID and 30 healthy controls) who had tested positive for COVID with the PCR test and conducted imaging scans of these patients within six months of subsequent PCR negative status. Average age of the cohorts was early 30s (note: this was a very young cohort). Eighteen individuals had been hospitalized with severe COVID-19 whereas five of the subjects reported moderate symptoms; the remaining 15 of the total 38 reported only mild symptoms. Loss of sense of smell (16/38), fatigue (72.41%), headache (44.83%), lack of attention (48.27%), issues with memory (31.03%), and lack of sleep (41.38%) were some of the most common lingering issues. Areas of damage in both the gray and white matter of the brain seen in the study included:
b .The inferior gyrus of the orbitofrontal lobe is linked to cognition Clusters found in the frontal lobes were connected to the white matter tracts which are the lines of communication (the brains superhighway system) including connections to the uncinate fasciculus tract. This tract connects the limbic and paralimbic regions with the orbito-frontal gyrus. The limbic, paralimbic and orbito-frontal regions play a central role in emotion processing. If connections are lacking here, this may be linked to mental health issues and reduced memory. c. Right orbital-inferior frontal gyrus (associated with various cognitive functions including attention, motor inhibition and imagery, as well as social cognitive processes). Note: The limbic system include structures between the cortex and the hypothalamus and brainstem, alone with the amygdala and hippocampus and the olfactory cortex. The hippocampi is essential to memory formation. The amygdala regulates emotions. The hypothalamus is responsible for regulating temperature, appetite, and communicates with our autonomic nervous system (which regulates things like heartbeat and blood pressure), endocrine system, and the viscera. 2. Midbrain/brainstem/right ventral diencephalonAbnormalities in the midbrain and pons have been connected to multiple symptoms of COVID like fatigue, insomnia, anxiety, depression, headaches, and cognitive problems. These regions are associated with many crucial bodily functions, including coordinating with the endocrine system to release hormones, relaying sensory and motor signals to the cerebral cortex and regulating circadian rhythms (the sleep-wake cycle). FATIGUE: It’s not all in your head. One of the most common and debilitating symptoms in long COVID is fatigue. The brain regions found affected in the SWI study also have been associated with fatigue in other neurodegenerative diseases. The study’s findings relevant to involvement of the frontal lobe and limbic and paralimbic regions correlate what has been found in other studies where fatigue was shown to be associated with higher functional connectivity between regions, including: the bilateral superior frontal gyri; the anterior cingulate gyrus; precuneus; right angular gyrus; posterior central gyrus; hippocampus; midbrain; supplementary motor area; posterior cingulate gyrus; and the thalamus. Over the last 20 years, an increasing number of studies have evaluated the pathogenetic bases of multiple sclerosis-related fatigue. Converging evidence from neurophysiology and neuroimaging research suggests that a dysfunction in a cortico-subcortical pathway, centered on thalamus, is involved in the pathogenesis of fatigue. Implications from this research. Long COVID patients have significant and prolonged effects on the brain, as seen on MRI with SWI scans. Those suffering with neurological symptoms of brain fog, cognitive issues, and other ongoing related problems should consider having this type of scan done to look for microscopic damage. In my opinion, this study also suggests that it is not always the severity of the viral infection taking center stage in this medical debacle, but it is the lingering viral remnants causing the downfall of the brain. Potentially, the most destructive elements are the residual and toxic effects of spike protein that can remain in the system after a COVID infection and following COVID vaccinations as well. Most researchers have found no definitive evidence of lingering whole virus as noted in this study published in the Annals of Internal Medicine, with many others that support the findings. For additional information, I encourage you to review the previous articles in our regularly updated long COVID series, including: https://www.suzannegazdamd.com/blog---long-covid/the-brain-under-attack-in-long-covid https://www.suzannegazdamd.com/blog---long-covid/the-smoking-gun-a-case-that-exemplifies-the-potential-harm-of-spike-protein-lingering-after-a-covid-vaccination https://www.suzannegazdamd.com/blog---long-covid/last-centurys-long-haulersback-again We know that spike protein has many downstream effects from micro-clotting, formation of prions, neuro-inflammation, autoimmune dysregulation, the formation of autoantibodies, destruction of white and gray matter, destruction of glial cells, microglial cell activation, impairing autophagy, mast cell activation, and other detrimental impacts. So, as scientists continue to acquire more understanding of the processes underlying long COVID, the role of spike protein likely will be further investigated – and ideally lead to more treatments and better patient outcomes. The “perfect” imperfect storm is upon us. In hope and healing, Dr. Suzanne Gazda References: Sapna S Mishra, Rakibul Hafiz, Rohit Misra, Tapan K. Gandhi, Alok Prasad, Vidur Mahajand, Bharat B. Biswal. Susceptibility-Weighted Magnetic Resonance Imaging Highlights Brain Alterations in COVID Recovered Patients. medRxiv. 2022.11.21.22282600; doi: https://doi.org/10.1101/2022.11.21.22282600 Van Bueskom, M. Global data reveal half may have long COVID 4 months on. Center for Infectious Disease Research and Policy. April 18, 2022. https://www.cidrap.umn.edu/news-perspective/2022/04/global-data-reveal-half-may-have-long-covid-4-months Verger, A., Kas, A., Dudouet, P. et al. Visual interpretation of brain hypometabolism related to neurological long COVID: a French multicentric experience. Eur J Nucl Med Mol Imaging 49, 3197–3202 (2022). https://doi.org/10.1007/s00259-022-05753-5 Douaud, G., Lee, S., Alfaro-Almagro, F. et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 604, 697–707 (2022). https://doi.org/10.1038/s41586-022-04569-5 Ludovica Brusaferri, Zeynab Alshelh, et al. The pandemic brain: Neuroinflammation in non-infected individuals during the COVID-19 pandemic. Brain, Behavior, Immunity. (2022) https://www.sciencedirect.com/science/article/pii/S0889159122000472#! Larsen JP, Britt W 3rd, Kido D, Olson BL, Holshouser BA, Kirsch WM. Susceptibility-Weighted Magnetic Resonance Imaging in the Evaluation of Dementia. Radiol Case Rep. 2015;2(4):102. Published 2015 Dec 7. doi:10.2484/rcr.v2i4.102 Lucas Scardua Silva, Rafael Batista Joao, et al. Functional and microstructural brain abnormalities, fatigue, and cognitive dysfunction after mild COVID-19. medRxiv. (2021) https://www.medrxiv.org/content/10.1101/2021.03.20.21253414v2 Clark AL, Sorg SF, Holiday K, et al. Fatigue Is Associated With Global and Regional Thalamic Morphometry in Veterans With a History of Mild Traumatic Brain Injury. J Head Trauma Rehabil. 2018;33(6):382-392. doi:10.1097/HTR.0000000000000377 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6066453/ Capone F, Collorone S, Cortese R, Di Lazzaro V, Moccia M. Fatigue in multiple sclerosis: The role of thalamus. Multiple Sclerosis Journal. 2020;26(1):6-16. doi:10.1177/1352458519851247 Michael C. Sneller, C. Jason Liang, Adriana R. Marques, et al. A Longitudinal Study of COVID-19 Sequelae and Immunity: Baseline Findings. Ann Intern Med. 2022;175:969-979. [Epub 24 May 2022]. doi:10.7326/M21-4905 Additional references: Conklin J, Frosch MP, Mukerji SS, et al. Susceptibility-weighted imaging reveals cerebral microvascular injury in severe COVID-19. J Neurol Sci. 2021;421:117308. doi:10.1016/j.jns.2021.117308 https://pubmed.ncbi.nlm.nih.gov/33497950/ Stefanos Klironomos, Antonios Tzortzakakis, Annika Kits, et al. Nervous System Involvement in Coronavirus Disease 2019: Results from a Retrospective Consecutive Neuroimaging Cohort Radiology 2020 297:3, E324-E334 https://pubs.rsna.org/doi/full/10.1148/radiol.2020202791 Oh J, Cho WH, Barcelon E, Kim KH, Hong J, Lee SJ. SARS-CoV-2 spike protein induces cognitive deficit and anxiety-like behavior in mouse via non-cell autonomous hippocampal neuronal death. Sci Rep. 2022;12(1):5496. Published 2022 Mar 31. doi:10.1038/s41598-022-09410-7 https://pubmed.ncbi.nlm.nih.gov/35361832/ Frank MG, Nguyen KH, Ball JB, et al. SARS-CoV-2 spike S1 subunit induces neuroinflammatory, microglial and behavioral sickness responses: Evidence of PAMP-like properties. Brain Behav Immun. 2022;100:267-277. doi:10.1016/j.bbi.2021.12.007 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8667429/
5 Comments
Vanessa Benke
12/24/2022 08:17:55 am
Once you’re able to determine through MRI or PET, scans and CT scans that a patient is in fact, having trouble due to long Covid and spike protein in the brain, what is the best recourse at this time? Is there anything one can do to help diminish further damage? What are current treatments ?
Reply
12/24/2022 10:34:53 am
Here is my answer
Reply
Kimberly Spangler
7/3/2023 03:34:31 pm
I am actually a patient at your Paesanos Parkway clinic, and have been corresponding with "my" doctor (from your clinic) regarding increased neurological symptoms I have been experiencing since my first dose of the covid vaccine in early 2021, and subsequently contracting covid the end of January 2022. I didn't make the connection to covid/the vaccine until I had my 5th dose this past October (10 days after my last dose, I became extremely ill, and have been housebound). I am not able to exert myself and have spent most of the past 9 months in bed. I wasn't offered testing to determine if in fact my extreme symptoms could ha e been induced by the vaccine and/or from when I had covid. My symptoms are debilitating and I am desperate for help! Is there a way for me to be seen by you, so we can try to address these concerns? I am currently on the schedule to see one of the PAs in your practice on 14 July.
Reply
Laura
9/16/2023 05:14:32 pm
Im sorry to see this doctor never replied. Wont be going with this office
Reply
M. Friesenhahn
9/17/2023 10:14:15 am
Dr. Gazda replies to her patients' comments/requests directly via email.
Reply
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorSuzanne Gazda M.D. Neurologist Archives
January 2024
Categories |

 RSS Feed
RSS Feed