|
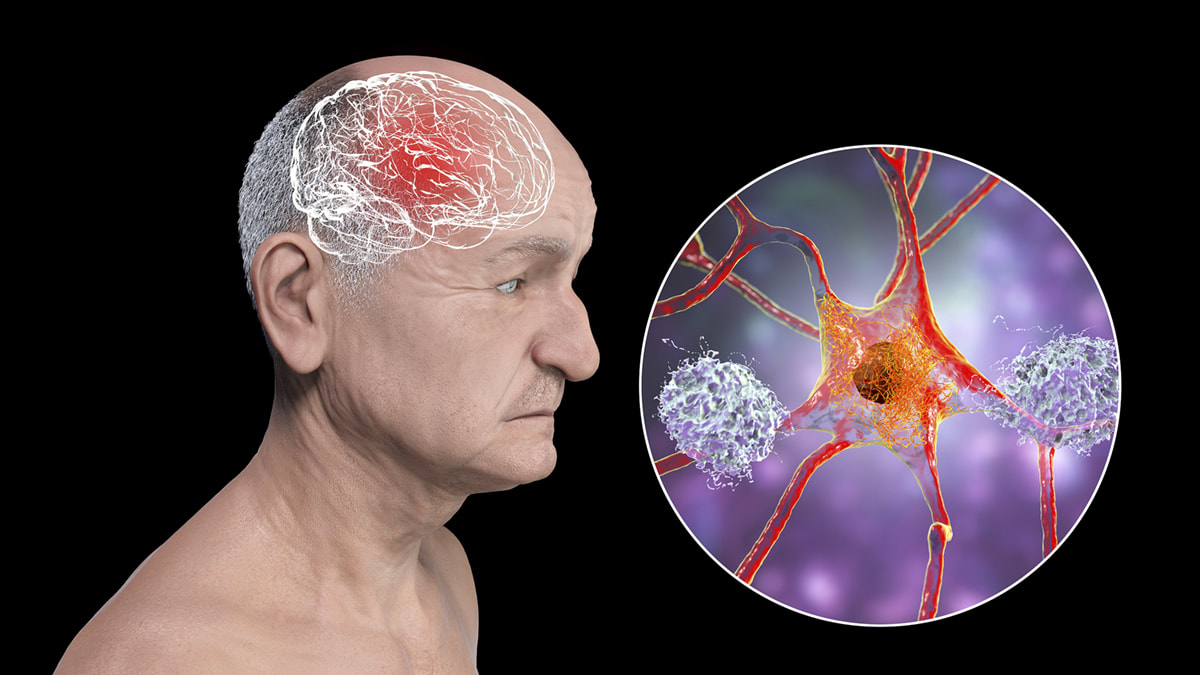
Up to two years after a COVID 19 infection, the risk of developing conditions such as psychosis, dementia, "brain fog," and seizures is still higher than after other respiratory infections, as reported in a study published recently in the Lancet Psychiatry.
We must ask:
Alzheimer's is a chronic, progressive neurodegenerative disease that affects at least 50 million people worldwide. The number of people living with Alzheimer's has increased dramatically since 1990 due to aging and population growth and is projected to exceed 152 million cases by 2050. Dr Dale Bredesen, a neurologist known for his work in improving cognitive decline in Alzheimer's disease, has said that Alzheimer's should be a RARE disease. He and other clinicians imply that there are many factors involved in deteriorating brain health, including the toxicity of our environment, obesity, a dramatic decline in metabolic health, etc.
I have warned that we are seeing and will continue to see a tsunami of neurodegenerative disease and that all projections pre-COVID regarding the incidence of neurodegenerative disease will exponentially rise. This article will discuss what appears to be a new form of Alzheimer's disease that is much more rapid in both onset and progression.
Past Lessons.
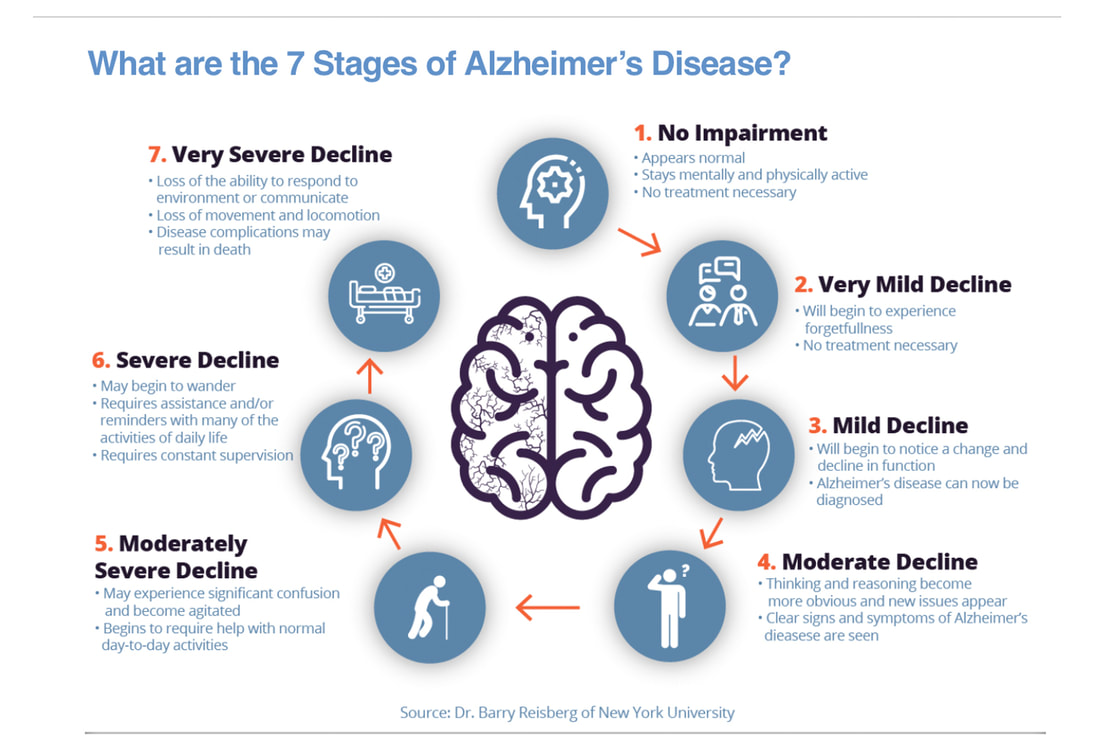
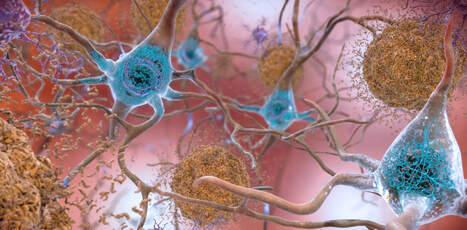
We have been taught that Alzheimer's disease and its associated changes in the brain can begin 20 years before symptoms appear, resulting from the slow accumulation of amyloid. The accumulation of amyloid is followed by the accumulation of hyperphosphorylated tau as many as 15-20 years before clinical symptoms emerge. This abnormal form of tau loses its ability to bind with microtubules, leading to the formation of neurofibrillary tangles, which are a biomarker of AD thought to be correlated with cognition. This progressive spread of tau precedes neurodegeneration and ultimately accompanies cognitive decline. Because amyloid and tau build up in the brain over many years, microglial cells (the brains innate immune cells) are activated resulting in neuroinflammation. This process is trying to correct the damage to neurons provoked by the buildup of amyloid and tau. Chronic neuroinflammation is the downfall of the brain. In most patients, there is typically a long period of time called the preclinical stage and then a step-wise decline that occurs over decades.
Once symptoms present, time is of the essence.
This short video provides an excellent explanation about some of the basics regarding Alzheimer's disease:
Shifting tides post COVID: has a new form of Alzheimer’s disease arrived?
Researchers are reporting a significant increase in Alzheimer’s disease post COVID that is much more rapid and progressive in onset then in times past. Dr. Luc Montagnier and his research team described a rapidly progressive form of Creutzfeldt-Jakob disease (CJD) unlike we have seen before, with onset of symptoms in less than two weeks of receiving a COVID vaccine; these patients died quickly within four to five months. CJD is a fatal prion disease that can be very difficult to diagnose with vague initial symptoms (memory loss, personality change, vision issues, and balance difficulties). Usually, death occurs within two years although some patients have slow progression and subclinical disease for a few years. In a study published July 2022 in the Journal of Alzheimer’s Disease, researchers report that people 65 and older who contracted COVID-19 were more prone to developing Alzheimer’s disease in the year following their COVID diagnosis. And the highest risk was observed in women at least 85 years old. The research team analyzed the anonymous electronic health records of 6.2 million adults 65 and older in the United States who received medical treatment between February 2020 and May 2021 and had no prior diagnosis of Alzheimer's disease. They then divided this population into two groups: one composed of people who contracted COVID-19 during that period, and another with people who had no documented cases of COVID-19. More than 400,000 people were enrolled in the COVID study group, while 5.8 million were in the non-infected group. The findings showed that the risk for developing Alzheimer's disease in older people nearly doubled (0.35% to 0.68%) over a one-year period following infection with COVID. The researchers say it is unclear whether COVID-19 triggers new development of Alzheimer's disease or accelerates its emergence. Either way, what we are seeing post COVID has never been seen before with this rapid onset of neurodegenerative disease. In a study by Tauqet and other researchers, 4.5 percent of older people developed dementia in the two years after infection, compared with 3.3 percent of the control group – this kind of rapid progression is unheard of until now.
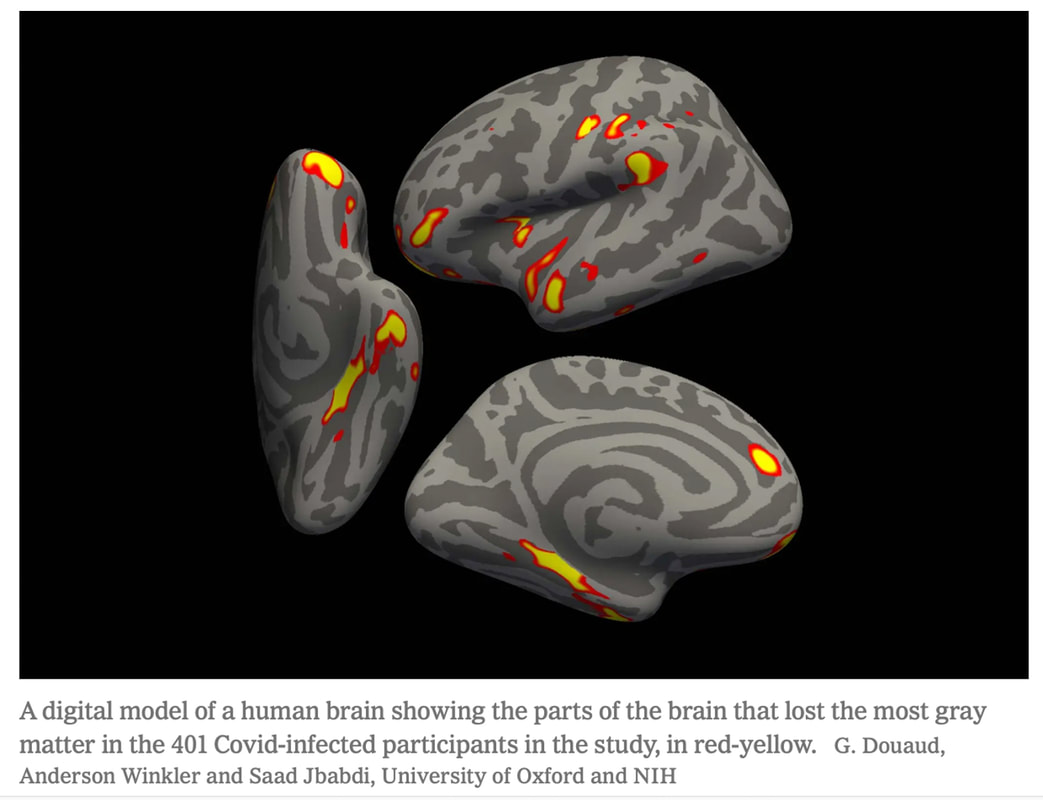
Credit: from the UK Biobank study
Earlier this year, the UK Biobank neuroimaging study showed that even mild COVID can lead to an overall reduction in the size of the brain, with notable effects in the frontal cortex, parahippocampal gyrus, and limbic system. These findings help explain the profound anxiety, depression, memory loss and executive dysfunction, trouble retrieving memories and other cognitive impairment experienced by so many long COVID patients.
More importantly, this same study suggests that the damage to the brain isn’t related to the severity of the infection. Structural and functional abnormalities of the brain can occur even in mild COVID cases. Because adults typically lose about 0.2 percent of their brain volume in regions related to memory every year, these findings translate to mental decline equivalent to 10 years of aging. This rapid decline in brain health is shocking as well. The study from Oxford showing lingering long-lasting neuropsychiatric symptoms in long COVID. In an analysis of retrospective cohort studies by seven scientists from Cambridge University and Oxford University in the United Kingdom more than 1.2 million patients each in the experimental and control groups were studied from multiple countries Of the 1,284,437 patients with the COVID-19 infection, their mean age was 42.5 years, ranging from children to the elderly. It was found that at six months of diagnosis, the risk of dementia was significantly higher in those who recovered from an infection with SARS COV2. 6 MONTHS!!!! And older adults diagnosed with dementia, brain fog, or epilepsy had mortality rates of 71 percent, 61 percent, and 83 percent, respectively, over the two-year follow-up period. And, a 2021 study of monkeys provided compelling evidence that the spike protein associated with SARS-CoV2 is responsible for Lewy body formation. Lewy bodies (LBs) are complex, intracellular inclusions that are common pathological features of many neurodegenerative diseases like Parkinson's and dementia. They consist largely of aggregated forms of the protein alpha-Synuclein (α-Syn), which misfolds to give rise to beta-sheet rich amyloid fibrils. For more about alpha-Synuclein, see my blog at: https://www.suzannegazdamd.com/scientifically-speaking1/alpha-synuclein-in-neurodegenerative-disease Spike-opathy: a new disease. This study published by Philip Oldfield in January 2022, is an excellent review on how SARS CoV 2 affects the brain, with an emphasis on the role of the spike protein in patients with neurological symptoms. Here is the abstract, edited lightly for clarity: "Following infection, patients with a history of neurological complications may be at a higher risk of developing long-term neurological conditions associated with the alpha-synuclein prion, such as Parkinson’s disease and Lewy body dementia. Compelling evidence has been published to indicate that the spike protein, which is derived from SARS-CoV-2 and generated from the vaccines, is not only able to cross the blood–brain barrier but may cause inflammation and/or blood clots in the brain. Consequently, should vaccine-induced expression of spike proteins not be limited to the site of injection and draining lymph nodes there is the potential of long-term implications following inoculation [vaccination] that may be identical to neurological complications seen in patients who were infected with SARS-CoV-2." And in this study, "Adverse effects of COVID-19 mRNA vaccines: the spike hypothesis," researchers offer an in-depth review of the many mechanisms of vaccination-mediated adverse effects (AEs) are reviewed from residual spike protein. Mechanisms of Injury to the Brain in Long COVID.
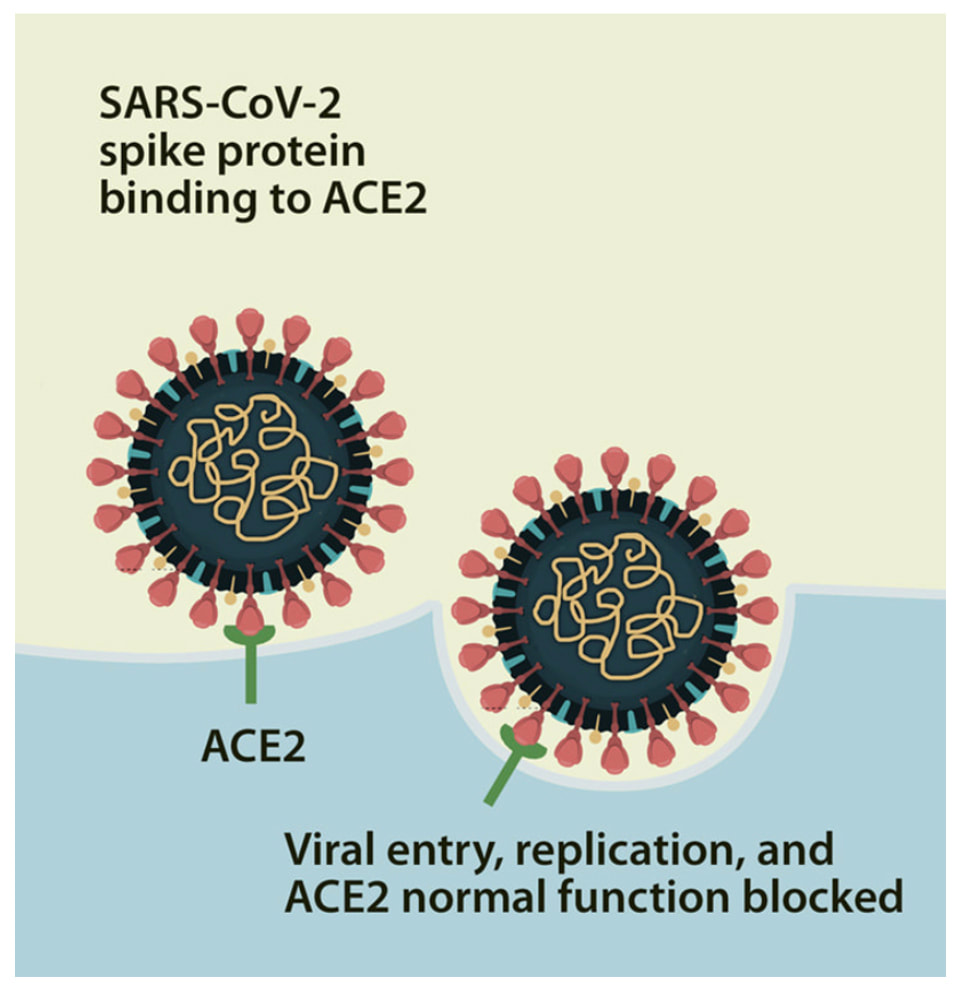
The BBB protects the central nervous system from toxins, pathogens, and other pro-inflammatory molecules. Spike proteins tested in vitro caused significant changes to the properties of the BBB with loss of barrier integrity. When the BBB is destabilized, the spike protein—and many other destructive substances—can freely pass into the brain, leading to the neurological complications seen in both those who have experienced the infection and those who have received a COVID vaccine.
In another study, the research team showed that spike protein all on its own and via pattern recognition acts as a pathogen to induce neuroinflammation. The Evidence is mounting: spike protein is a very toxic and lingering. This article, "Circulating SARS-CoV-2 Vaccine Antigen Detected in the Plasma of mRNA-1273 Vaccine Recipients" clearly lays out the ramification of the COVID shots on brain tissue: "These data show that S1 antigen production after the initial vaccination can be detected by day one and is present beyond the site of injection site and the associated regional lymph nodes." It was observed that the spike protein S1 subunit was detectable in the systemic circulation up to approximately two weeks post-injection in eleven out of thirteen healthcare workers. Although concentration of the S1 subunit was low, this study provides proof-of-principle that spike proteins can get into circulation following inoculation." And multiple other studies have shown that spike protein is not being cleared and can linger sometimes for over a year in monocytes, plasma, in exosomes, on thrombi and various other tissues sites. Just some of these studies include: Immune-Based Prediction of COVID-19 Severity and Chronicity Decoded Using Machine Learning Patterson et al Front Immunology 2021 Cutting Edge: Circulating Exosomes with COVID Spike Protein Are Induced by BNT162b2 (Pfizer–BioNTech) Vaccination prior to Development of Antibodies: A Novel Mechanism for Immune Activation by mRNA Vaccines Bansai et al The Journal of Immunology Evidence of SARS-CoV-2 spike protein on retrieved thrombi from COVID-19 patients De Michelle M et al Journal of Hematology & Oncology August 2022 Persistent circulating SARS-CoV-2 spike is associated with post-acute COVID-19 sequelae Swank Z et al medRxiv pre-print June 2022 Persistent varicella zoster virus infection following mRNA COVID-19 vaccination was associated with the presence of encoded spike protein in the lesion Yamamoto M Cutaneous Immunology August 2022 Persistent Circulation of Soluble/EV-linked Spike Protein and Viral RNA in Individuals with Post-Acute Sequelae of COVID-19 Craddock V et al The Lancet Preprint August 2022 Clinical and Molecular Characterization of a Rare Case of BNT162b2 mRNA COVID-19 Vaccine-Associated Myositis, Vaccines. July 2022 I have reviewed what I call The Five Horsemen of injury to the brain and central nervous system. In brief, we see:
Other responsible mechanisms also include: a. High levels of oxidative stress Oxidative stress and inflammation are mutually reinforcing each other, The brain, with its high oxygen consumption and lipid-rich content, is highly susceptible to oxidative stress. Oxidative stress is involved in neurodegenerative disorders such as Alzheimer disease, Huntington disease, and Parkinson disease etc. b. Mitochondrial dysfunction
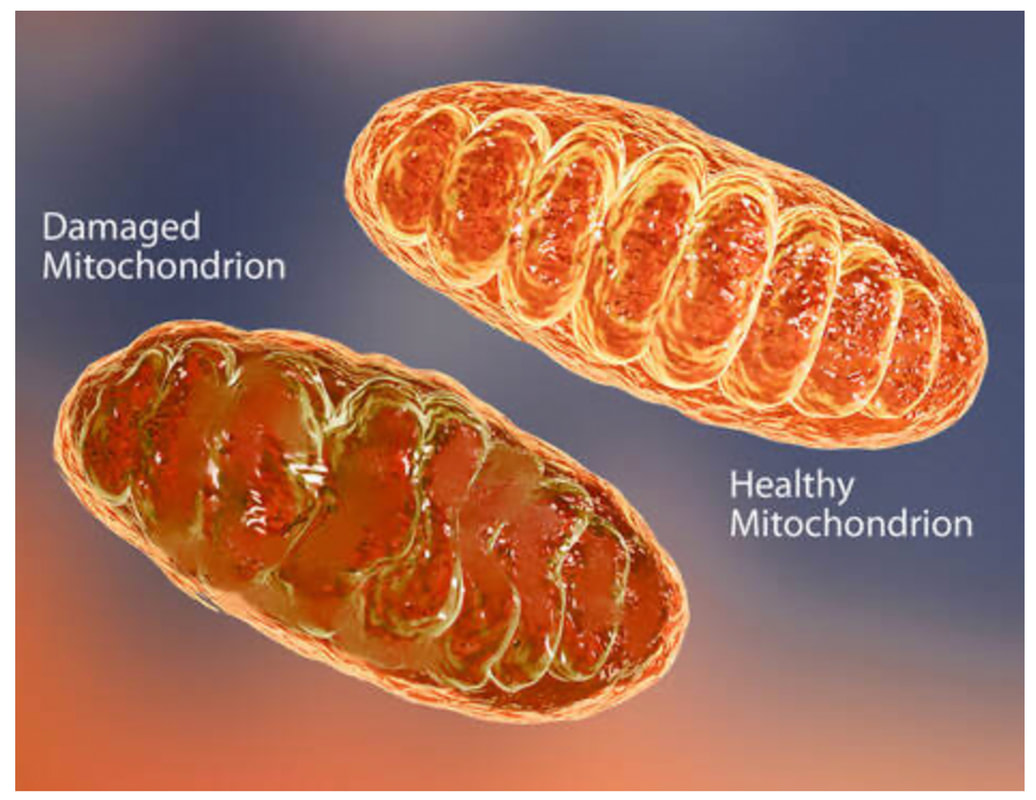
In April 2021, a study published in Circulation Research found that spike proteins disrupt the structure and functions of mitochondria in cells. Mitochondrial dysfunction occurs in neurodegenerative disease and a large body of evidence suggests that damaged mitochondria likely play fundamental roles in the pathogenesis of AD.
c. Advanced Senescence
d. Gut microbiome imbalance
The beneficial immune modulating microbiota in the gut microbiome have been shown to have been affected after a COVID illness. Spike protein damages the microbiome as noted in this study by binding to bacterial lipopolysaccharide and boosting pro-inflammatory activity.
Research suggests that the human microbiome gut dysbiosis could be a risk factor for neurodegenerative disease.
d. Damage to DNA
DNA damage and defective DNA repair are now increasingly implicated in age- related neurodegenerative diseases.
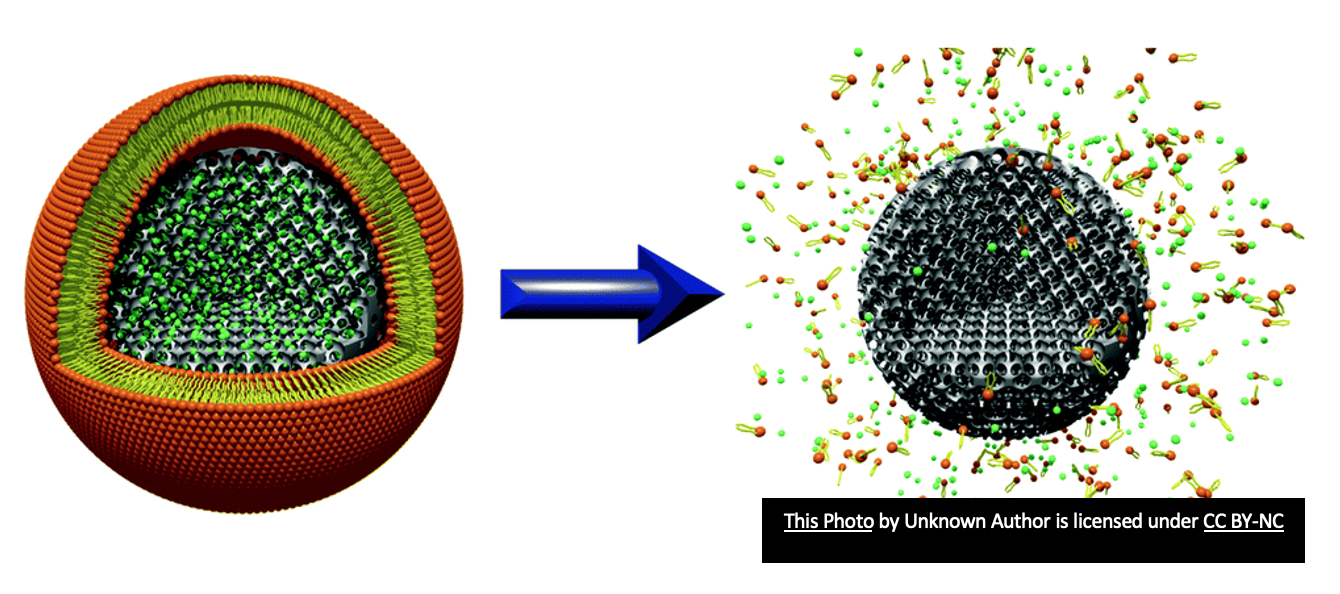
In a study published in the journal Viruses, laboratories from two Swedish universities reported that spike proteins would inhibit the ability of growing cells to repair DNA damages. And in this study, mRNA was found to reverse transcribe into DNA which could therefore alter one’s genome. f. Altered Epigenetics The aging process is regulated by epigenetic factors. Epigenetic modifications have been found to be important players in the pathogenesis of Alzheimer's disease (AD), which is the most common type of dementia. Extensive research has suggested DNA methylation plays an important role in the course and development of AD. A genome-wide DNA methylation study published in April 2022 in the journal Nature Communications collected whole blood samples from 232 healthy individuals, 194 non-severe COVID-19 patients and 213 severe COVID-19 patients. Researchers discovered that the epigenetic age of COVID-19 patients was significantly accelerated. This result may shed some light on the fact that the COVID-19 infection can make our brain age by two decades. g. Lipid Nanoparticles Some wonder if the lipid nanoparticles (the substance surrounding the genetic message being delivered with COVID vaccinations) could lead to an increased risk of neurodegenerative disease.
Unique Shared Pathological Mechanisms in long COVID and Alzheimer's
A. ACE 2 Receptors The SARS CoV 2 virus uses spike protein to attach to ACE 2 receptors and infect cells ACE 2 receptors exist all over our body and brain and any ACE 2 receptor is a potential target for spike protein that is lingering post infection and post vaccine. AC2 is neuroprotective and if downregulated or blocked by S1, the neuroprotection is lost Decreased ACE2 activity is associated with increased activity in TGF-beta which fuels amyloid production & hyperphosphorylation of tau which results are associated with NDG.
B. Prions being spawned
Study: Neurotoxic Amyloidogenic Peptides Identified in the Proteome of SARS-COV2: Potential Implications for Neurological Symptoms In COVID-19.
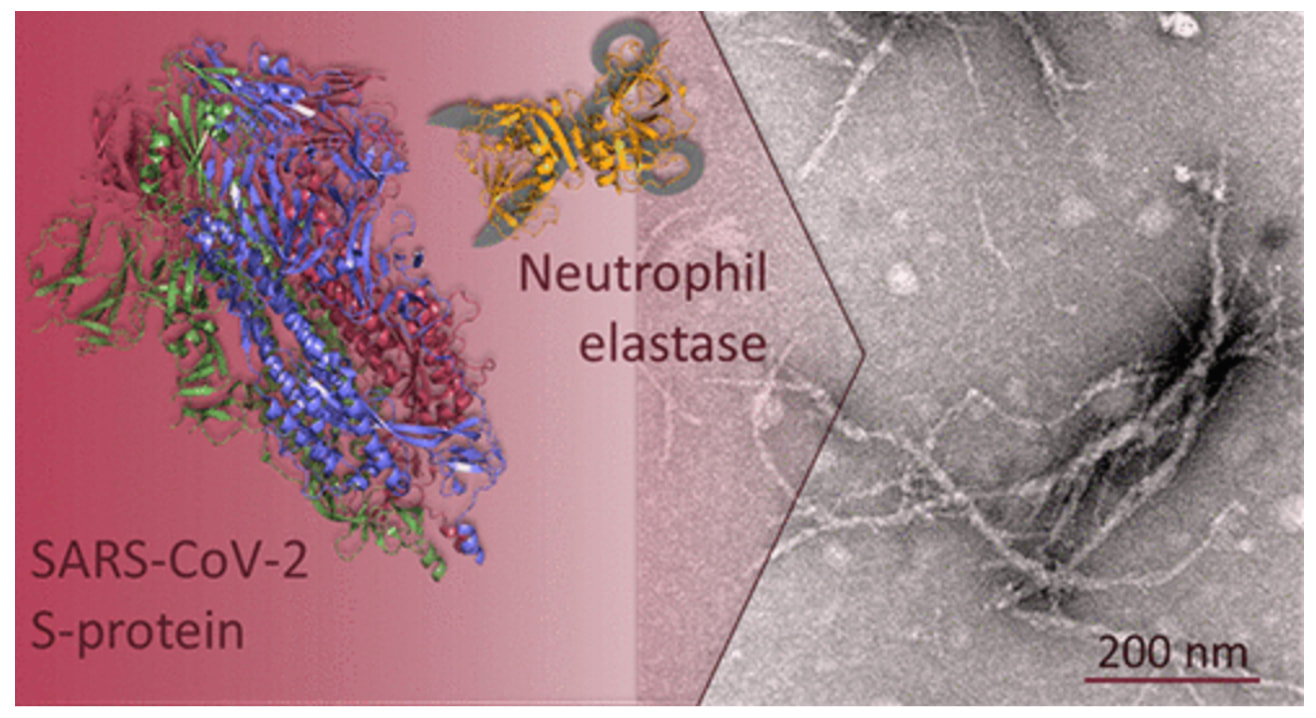
Spike protein is driving the production of prions which is misfolded protein that can cause disease by triggering normally healthy proteins in the brain to abnormally fold. Prions can self-propagate from cell-to-cell transfer and can spread via exosomes and they are resistant to proteolysis. A hallmark of neurodegenerative disease is the formation of misfoldedprotein aggregates that cause cellular toxicity.
SARS CoV 2 is the only coronavirus that contains in its receptor binding domain a prion arm. And as I previously noted, a recent study by Dr. Luc Montaigne et al showed prions present in all COVID vaccines and all variants except Omicron. The study by Nystrom showed that spike protein when placed in cell culture quickly transformed into amyloid fibrils.
From Amyloidogenesis of SARS-CoV-2 Spike Protein Nystrom S et al May 2022 Journal of American Chemical Society
And in another study, they found two highly amyloidogenic proteins of SARS CoV 2 in the ORF 6 and 10 (ORF stands for open reading frame, which are viral fragments). The authors stated "This pathology could be implicated in neuro Long COVID and could represent future risk of neurodegenerative disease." We know that amyloid can prompt other proteins to misfold in the brain via prion mechanisms and both amyloid and tau are the two pathological hallmarks of Alzheimer's disease.
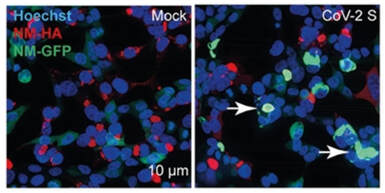
This post viral and post-vaccine production of amyloid is being fueled in the body and in the brain. The micro clots seen in long COVID contain an amyloid/fibrin combination making them very difficult for the body to break down. The question then becomes if amyloid is being formed and since amyloid is a prion, is it possible to turn off this process once it’s initiated? C. Spike protein activates the NLRP3 inflammasome NLRP3 is a critical component of the innate immune system that mediates proinflammatory cytokines in response to infection or cellular damage. This activation will promote tau hyperphosphorylation and the formation of neurofibrillary tangles; tau is one of the pathological hallmarks of Alzheimer's disease. Microglial NLRP3 inflammasome activation is a major driver of neurodegeneration. D. Exosomes carrying spike protein, viral fragments, and prions to faraway places Exosomes are defined as signaling organelles involved in health or in disease signaling pathways, cellular waste management and do contribute to the development of neurodegenerative disease. Spike protein has been found in exosomes post vaccination. Exosomes easily cross in and out of the brain and in the case of AD, the presence of exosomes containing tau or amyloid-β peptide has been reported. Here are two studies showing exosomes propagating prions in long COVID: In this study by Liu et al, exosomes were found to be assisting in the transfer of 2 viral fragments, VSV-G and the SARS-CoV2 S1 spike protein. When, spike protein was put in a cell culture, a dramatic boost of misfolded tau was formed. They found transfer of prions between cells via secretion of exosomes and or direct cell to cell contact. These mis-folded proteins self-propagate through the brain.
Remember, spike protein AND exosomes easily cross the blood-brain barrier. This process is likely going on in the body and the brain. We should NOT have amyloid, tau or other prions forming.
And, in this study done at University of California San Francisco, "SARS-CoV-2 and Mitochondrial Proteins in Neural-Derived Exosomes of COVID-19," clinicians surveyed 46 previously infected patients with 32 physical long-COVID symptoms. Additionally, they were experiencing mental health symptoms such as loss of memory, irritability, agitation, depression, anxiety, post-traumatic stress, and specific sensory losses and looked at neuron derived extracellular vesicles (NDEV).
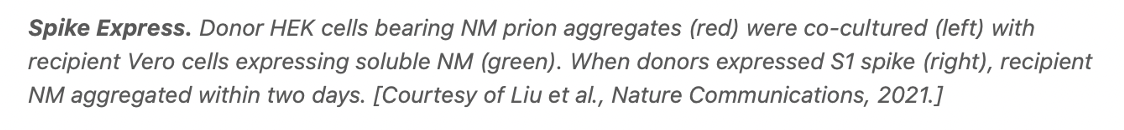
E. Spike protein harbors a heparin binding domain
F. Spike protein prevents clearing of amyloid
As noted in the study, "The effects of Aβ(1–42) binding to the SARS-CoV-2 spike protein S1 subunit and angiotensin-converting enzyme 2" Aβ1–42 (the 42 amino acid form of amyloid β in cerebrospinal fluid) was found to bind with high affinity to the S1 subunit and ACE2 with the task to increase viral entry. Data from a surrogate mouse model with IV inoculation of Aβ1–42 showed that the clearance of Aβ1–42 in the blood was dampened in the presence of the extracellular domain of the S protein trimers. G. Alzheimer’s Signaling in COVID Brains Additionally, in this study, high levels of oxidative stress post COVID were seen in the cortex and cerebellum. This caused calcium ions to leak from ion channels in the brain, known as ryanodine receptors and led to tau hyperphosphorylation and amyloid beta to form after COVID The study authors said that this study "shows that long COVID-19 brain fog may be a form of Alzheimer's disease."
Closing remarks.
I have warned that we will see a tsunami of neurodegenerative disease, the might of which we could not have imagined. Never before has humanity faced the health challenges that we are facing now and expect to confront going forward. As of today, according to Our World in Data, 67.9 percent of the world population has received at least one dose of a COVID-19 vaccine. A new disease has now emerged called "Spike-opathy." Concerns are building as to not just the short-term risk of lingering spike protein, but long term risks as well. No clinical trials were done to study this potential harm, and, as I have said before, "We are the clinical trial." We have learned in this blog that long COVID patients and patients with post-vaccine injuries who harbor residual spike protein can share many pathological mechanisms with Alzheimer's disease. With Alzheimer’s disease, changes in the brain can begin decades before symptoms appear, but now it appears we have a new more rapidly progressive form of this dreaded disease. If we understand the complex mechanisms of injury of Long COVID and post-vaccine injury, the mystery of brain fog and other spike protein-induced neurological problems will begin to lift. It seems more important than ever to truly see the landscape in front of us so that we learn more and come together as one to heal humanity. In hope and health, Dr. Suzanne Gazda For more information, see our full long COVID series at: https://www.suzannegazdamd.com/blog---long-covid References: Guo P, Benito Ballesteros A, Yeung SP, Liu R, Saha A, Curtis L, Kaser M, Haggard MP and Cheke LG (2022) COVCOG 2: Cognitive and Memory Deficits in Long COVID: A Second Publication From the COVID and Cognition Study. Front. Aging Neurosci. 14:804937. doi: 10.3389/fnagi.2022.804937 Taquet, M. et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. The Lancet Psychiatry. August 17, 2022. https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(22)00260-7/fulltext Matias-Guiu JA, Delgado-Alonso C, Yus M, et al. "Brain Fog" by COVID-19 or Alzheimer's Disease? A Case Report. Front Psychol. 2021;12:724022. Published 2021 Nov 4. doi:10.3389/fpsyg.2021.724022. https://pubmed.ncbi.nlm.nih.gov/34803804/ 2022 Alzheimer's disease facts and figures. Alzheimers Dement. 2022;18(4):700-789. doi:10.1002/alz.12638. https://pubmed.ncbi.nlm.nih.gov/35289055/ Wang, W. et al. Mitochondria dysfunction in the pathogenesis of Alzheimer's disease: recent advances. Molecular Neurodegeneration. 2020. https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-020-00376-6 Montagnier, L. et al. Towards the emergence of a new form of the neurodegenerative Creutzfeldt-Jakob disease: Twenty -six cases of CJD declared a few days after a COVID-19 Vaccine. Research Gate. Preprint June 2022 Meyer, K. et al. SARS-CoV-2 Spike Protein Induces Paracrine Senescence and Leukocyte Adhesion in Endothelial Cells. ASM Journals Journal of Virology Vol. 95, No. 17 August 2021 Rizou, S. et al. Ageing, Cellular Senescence and Neurodegenerative Disease. Internal J of Molecular Science 2018 Oct; 19 Giannos, P. et al. Gut dysbiosis and long COVID‐19: Feeling gutted. Med Virology. 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9088471/ Chen, C. et al. Gut microbiota regulate Alzheimer’s disease pathologies and cognitive disorders via PUFA-associated neuroinflammation. BMJ 2021 https://gut.bmj.com/content/early/2022/01/10/gutjnl-2021-326269 Bredesen, D., Sharlin, K. et al. Reversal of Cognitive Decline: 100 Patients. Journal of Alzheimer’s Disease & Parkinsonism. (2018) https://www.researchgate.net/publication/329063941_Reversal_of_Cognitive_Decline_100_Patients Aldén M, Olofsson Falla F, Yang D, Barghouth M, Luan C, Rasmussen M, De Marinis Y. Intracellular Reverse Transcription of Pfizer BioNTech COVID-19 mRNA Vaccine BNT162b2 In Vitro in Human Liver Cell Line. Current Issues in Molecular Biology. 2022; 44(3):1115-1126. https://doi.org/10.3390/cimb44030073 Choi Y et al. Nanoparticles for gene delivery: therapeutic and toxic effects. Molecular & Cellular Toxicology. volume 10, pages 1–8 (2014) Sweeney P, Park H, Baumann M, et al. Protein misfolding in neurodegenerative diseases: implications and strategies. Transl Neurodegener. 2017;6:6. Published 2017 Mar 13. doi:10.1186/s40035-017-0077-5 Tetz G, Tetz V. Prion-like Domains in Spike Protein of SARS-CoV-2 Differ across Its Variants and Enable Changes in Affinity to ACE2. Microorganisms. 2022;10(2):280. Published 2022 Jan 25. doi:10.3390/microorganisms10020280. https://pubmed.ncbi.nlm.nih.gov/35208734/ Charnley, M. et al. Neurotoxic amyloidogenic peptides in the proteome of SARS CoV 2: Potential for neurological symptoms in COVID 19. Nature Communications. March 2022 Albornoz, E. SARS-CoV-2 drives NLRP3 inflammasome activation in human microglia through spike-ACE2 receptor interaction. bioRxiv (preprint Jan 2022) https://www.biorxiv.org/content/10.1101/2022.01.11.475947v1 Idrees D, Kumar V. SARS-CoV-2 spike protein interactions with amyloidogenic proteins: Potential clues to neurodegeneration. Biochem Biophys Res Commun. 2021;554:94-98. doi:10.1016/j.bbrc.2021.03.100 Nyström S, Hammarström P. Amyloidogenesis of SARS-CoV-2 Spike Protein. J Am Chem Soc. 2022;144(20):8945-8950. doi:10.1021/jacs.2c03925 Peluso MJ, Deeks SG, Mustapic M, et al. SARS-CoV-2 and Mitochondrial Proteins in Neural-Derived Exosomes of COVID-19. Ann Neurol. 2022;91(6):772-781. doi:10.1002/ana.26350 Rhea EM, Logsdon AF, Hansen KM, et al. The S1 protein of SARS-CoV-2 crosses the blood-brain barrier in mice. Nat Neurosci. 2021;24(3):368-378. doi:10.1038/s41593-020-00771-8 Mia, G. ORF3a of the COVID-19 virus SARS-CoV-2 blocks HOPS complex-mediated assembly of the SNARE complex required for autolysosome formation. Developmental Cell, Dec 2020. P427-442.E5 Liu, S. Highly efficient intercellular spreading of protein misfolding mediated by viral ligand-receptor interactions. Nat Commun. 2021 Oct 19;12(1):5739. Villa, C et al Can SARS-CoV-2 Infection Exacerbate Alzheimer’s Disease? An Overview of Shared Risk Factors and Pathogenetic Mechanisms. J. Pers. Med. 2022 Folbracht, C. et al. Oxidative Stress and Hyper-Inflammation as Major Drivers of Severe COVID-19 and Long COVID: Implications for the Benefit of High-Dose Intravenous Vitamin. Front Pharmacol. 2022; Apr 29. doi: 10.3389/fphar.2022.899198 Ganna Petruk, Manoj Puthia, Jitka Petrlova, Firdaus Samsudin, Ann-Charlotte Strömdahl, Samuel Cerps, Lena Uller, Sven Kjellström, Peter J Bond, and Artur Schmidtchen, SARS-CoV-2 spike protein binds to bacterial lipopolysaccharide and boosts proinflammatory activity, Journal of Molecular Cell Biology, Volume 12, Issue 12, December 2020, Pages 916–932, https://doi.org/10.1093/jmcb/mjaa067 Aisen P., Cummings J., Jack, CR Jr., et al. On the path to 2025: understanding the Alzheimer's disease continuum. 2017;9(1):1-10 Selkoe DJ. Hardy J. The amyloid hypothesis of Alzheimer's disease at 25 years. EMBO Mol Med.2016;8(6):595-608 Agrawal M. 2020;447-460. Molecular basis of chronic neurodegeneration. 10.1016/B978-0-12-809356-6.00026-5 Alzheimer’s Disease Fact Sheet. National Institute on Aging. Updated July 08, 2021. Accessed June 16, 2022. https://www.nia.nih.gov/health/alzheimers-disease-fact-sheet. Alzheimer’s Disease International. 2018. World Alzheimer Report 2018. London: Alzheimer's Disease International. Jiang Hu et al. SARS-CoV-2 Spike Impairs DNA Damage Repair and Inhibits V(D)J Recombination In Vitro. Viruses. 2021 Oct 13;13(10):2056. Hsu JT, Tien CF, Yu GY, et al. The Effects of Aβ1-42 Binding to the SARS-CoV-2 Spike Protein S1 Subunit and Angiotensin-Converting Enzyme 2. Int J Mol Sci. 2021;22(15):8226. Published 2021 Jul 30. doi:10.3390/ijms22158226 Trougakas, I. Adverse effects of COVID-19 mRNA vaccines: the spike hypothesis. Trends in Molecular Medicine. April 20, 2022. https://www.cell.com/trends/molecular-medicine/fulltext/S1471-4914(22)00103-4#bb0470 Alden et al. Intracellular Reverse Transcription of Pfizer BioNTech COVID-19 mRNA Vaccine BNT162b2. In Vitro in Human Liver Cell Line. Biology. Jan 2022. Highly efficient intercellular spreading of protein misfolding mediated by viral ligand-receptor interactions. Liu S Nat Commun. 2021 Oct 19;12(1):5739.) Inside the Brain Part 2. Alzheimer's Association. Accessed June 16, 2022. https://www.alz.org/alzheimers-dementia/what-is-alzheimers/brain_tour_part_2 Alzheimer’s Association. Stages of Alzheimer's. https://www.alz.org/alzheimers-dementia/stages. Accessed 1 December 2020. How Biomarkers Help Diagnose Dementia. National Institute on Aging. Updated January 21, 2022. https://www.nia.nih.gov/health/how-biomarkers-help-diagnose-dementia). Rabinovici GD, Gatsonis C, Apgar C, et al. Association of amyloid positron emission tomography with subsequent change in clinical management among Medicare beneficiaries with mild cognitive impairment or dementia. JAMA. 2019;321(13):1286-1294. Clough, E. et al. Mitochondrial Dynamics in SARS-COV2 Spike Protein Treated Human Microglia: Implications for Neuro-COVID. J Neuroimmune Pharmacol. 2021
2 Comments
Kristina
10/30/2022 03:45:52 am
!!!!
Reply
Brenda Dick
5/7/2023 09:45:20 pm
Please can I speak with someone? My dad is having these symptoms- had covid- was hospitalized and now we are seeing the scary onset of what they believe is Lewy dementia and Parkinson like symptoms. We are going to Hershey medical center tom. but would love more guidance. Can you help? 814-660-9458.. Thank you.
Reply
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorSuzanne Gazda M.D. Neurologist Archives
January 2024
Categories |



 RSS Feed
RSS Feed