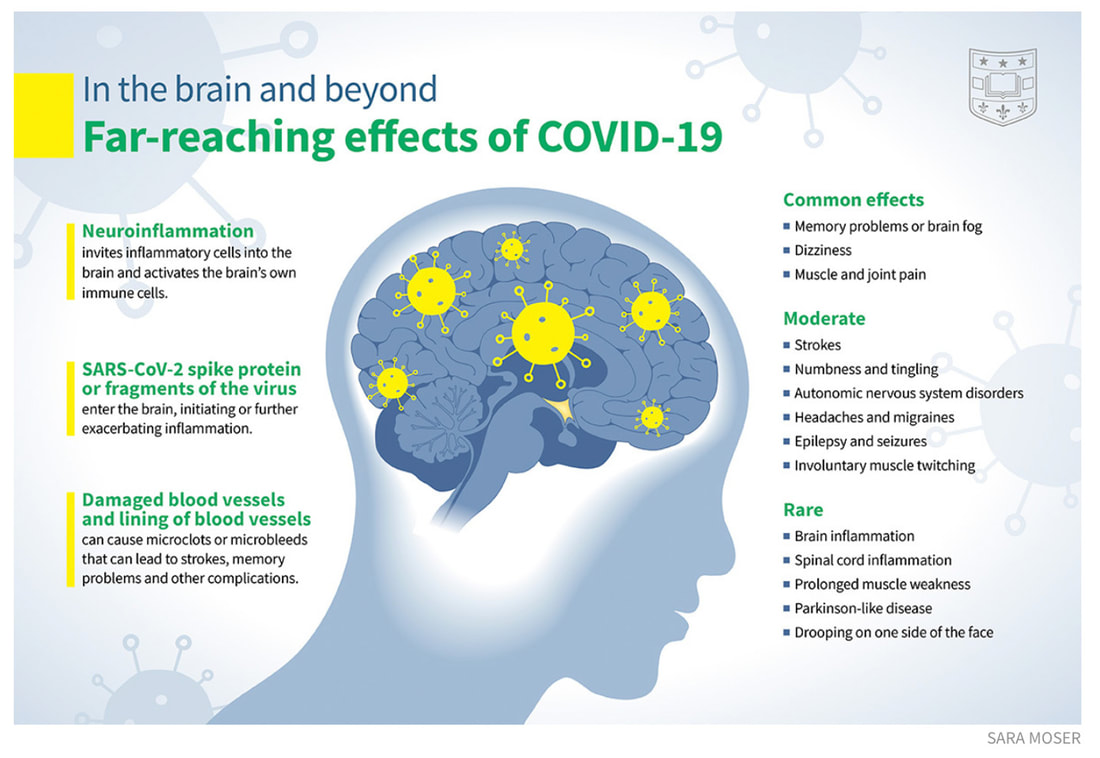
As it stands now, and noted in a recent cohort study, it is estimated that one in eight adults (12.7%) diagnosed with COVID-19 will likely experience long-term symptoms. One of this large study's authors, Aranka Ballering of the Dutch University of Groningen, stated that long COVID was "an urgent problem with a mounting human toll." Her observations and sentiments have been echoed by numerous physicians who are seeing in both their research as well as in clinical settings that more and patients are continuing to experience debilitating symptoms long after the initial virus has subsided. And as we’ve previously noted, neurological issues are cited by many as causing a great deal of distress. In fact, another investigation released this year stated that brain fog and cognitive effects are being seen in as many of 70% of patients diagnosed with this complex syndrome. Long, long, long COVID. A recent analysis from Cambridge University and Oxford University, United Kingdom, scanned electronic medical records of approximately 89 million patients and identified more than 1.28 million cases of COVID-19 infection, and matched them to a cohort of non-COVID patients who were suffering from other respiratory infections. The results showed an astounding persistence of increased risk of psychotic disorder, cognitive deficit, dementia, and epilepsy lingering 2 years post infection And there’s more…another remarkable evalution, published in Nature Medicine, assessed brain health in veterans across 44 different disorders for a period of a year post infection. The methodology included data sets of 154,000 people who had tested positive for COVID-19 sometime between March 1, 2020 and January 15, 2021. These subjects were studied versus a control group of more than 5.6 million patients who did not have COVID-19 during the same time frame, and a control group of more than 5.8 million people from March 2018 to December 31, 2019 (the period prior to COVID). The researchers examined brain health over a year from the date of diagnosis of infection. It’s important to note that vaccination history was not examined and given that this was a large population of veterans, it’s possible to assume that many patients in this study likely received a COVID vaccination during this same timeframe. Credit: https://medicine.wustl.edu/news/covid-19-infections-increase-risk-of-long-term-brain-problems/ The noted neurological effects post-COVID infection.
In this extensive analysis it was determined that brain and other neurological disorders occurred in 7% more of those who had been infected with COVID compared with a similar group of veterans who had never been infected. That translates into roughly 6.6 million Americans who had brain impairments within one year.
Two key points must be highlighted:
In summary: the brain and the central nervous system are being hit very, very hard post COVID and in post-vaccine injury as well. I previously have spoken about the tremendous number of reported adverse events following administration of COVID vaccinations, including at this writing over 1.5 million injuries and more than 30,000 deaths as submitted to the Vaccine Adverse Events Reporting System (VAERS). The World Council for Health organization also provides regularly updated information and commentary by leading clinicians in the field. For additional related reading about the link between long COVID and post-vaccine injuries, please see my blog in our extensive series at: https://www.suzannegazdamd.com/blog---long-covid/will-we-see-a-rise-in-neurodegenerative-disease-post-covid-and-post-covid-vaccines There has been growing concern as to whether cognitive deficits will remain for years as a chronic syndrome, and whether patients will experience neurodegeneration and dementia in the long-term, despite recovery of other acute and sub-acute symptoms. This study is just one of many that examines the potential for lingering issues that is yet to be known, but will continue to be researched at length. Coming up in my next blog, I will discuss further the identified rise in Alzheimer’s disease and the shared pathology between long COVID and viral fragments from lingering spike protein, which is the most toxic protein known to date. We are facing a tsunami of health impacts because of SARS-CoV-2 and lingering spike protein. I encourage you to please see my prior blogs in our extensive long COVID series to learn more and don’t hesitate to reach out if we can help. In health and hope, Dr. Suzanne Gazda References: Guo P, Benito Ballesteros A, Yeung SP, Liu R, Saha A, Curtis L, Kaser M, Haggard MP and Cheke LG (2022) COVCOG 2: Cognitive and Memory Deficits in Long COVID: A Second Publication From the COVID and Cognition Study. Front. Aging Neurosci. 14:804937. doi:10.3389/fnagi.2022.804937 https://www.frontiersin.org/articles/10.3389/fnagi.2022.804937/full Ballering, A. et al. Persistence of somatic symptoms after COVID-19 in the Netherlands: an observational cohort study. The Lancet. August 6, 2022. https://doi.org/10.1016/S0140-6736(22)01214-4. https://www.frontiersin.org/articles/10.3389/fnagi.2022.804937/full Taquet M, Sillett R, Zhu L, et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. Lancet Psychiatry. 2022;9(10):815-827. doi:10.1016/S2215-0366(22)00260-7 https://pubmed.ncbi.nlm.nih.gov/35987197/ Xu, E., Xie, Y. & Al-Aly, Z. Long-term neurologic outcomes of COVID-19. Nat Med (2022). https://doi.org/10.1038/s41591-022-02001-z Miners S, Kehoe PG, Love S. Cognitive impact of COVID-19: looking beyond the short term. Alzheimers Res Ther. 2020;12(1):170. Published 2020 Dec 30. doi:10.1186/s13195-020-00744-w https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7772800/ Vaccine Adverse Event Reporting System https://vaers.hhs.gov/ World Council for Health https://worldcouncilforhealth.org/
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorSuzanne Gazda M.D. Neurologist Archives
January 2024
Categories |
 RSS Feed
RSS Feed