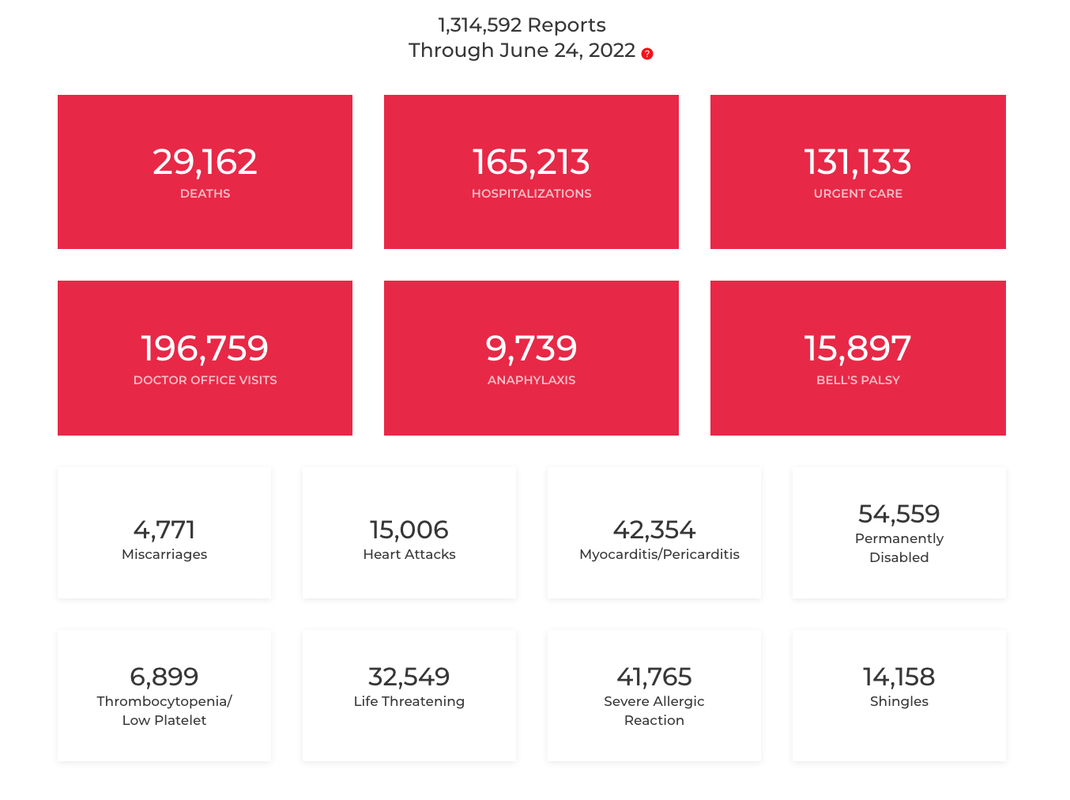
Additional reports note that more Americans in and out of the labor force are having trouble remembering and concentrating, experiencing overwhelming fatigue, shortness of breath, exercise intolerance, neuropathic and muscle pain, weakness, and a long list of other symptoms. And that despite a strong job market, with the number and rate of job openings at all-time highs, applications for Social Security Disability Insurance are (slowly) rising again in their first sustained increase since 2009. Regarding post-vaccine complications, figures from the Vaccine Adverse Event Reporting System (VAERS) as of June 10, 2022, show over 28,000 deaths and 129,5327 adverse reports that have been submitted for review and verification. Some basic definitions Long COVID Experts note that while recovery times for an initial COVID infection can vary, long COVID refers to instances where symptoms persist for 90+ days. Long COVID is generally diagnosed when signs and symptoms of COVID that can't be explained by other causes are present four weeks after the initial infection. Long COVID prevalence among hospitalized patients was 54%. Approximately 25 to 35% or more of all patients who have had COVID are experiencing at least some of these long-hauler symptoms in varying degrees of severity. Up to 80% of patients may have some long-lasting symptom. Long COVID tends not to be related to the severity of COVID.
Since Phase 3 and Phase 4 clinical trials are still ongoing, the full safety and toxicity profile for COVID-19 vaccines cannot be fully determined. From a bioethical perspective, cases of any new-onset or worsened signs, symptoms, or abnormalities following any dose of COVID-19 vaccine must be considered as an injury caused by the vaccine, until proven otherwise. Patients with post-vaccine injury should not receive additional COVID vaccines. There are significant overlaps between the symptoms and features of long COVID/long-hauler syndrome and post-vaccine syndrome. However, several clinical features appear to be characteristic of post-vaccine syndrome; most notably, severe neurological symptoms appear to be more common following vaccination. To complicate matters further, patients with long COVID are often also vaccinated, making the issue of definition more difficult. For the purposes of treatment or other discussions, we will refer to both disease states as long-haul COVID 19 syndrome (LHCS).
To read more about the mechanisms that may contribute to autoantibody formation: https://www.science.org/content/article/rare-cases-coronavirus-vaccines-may-cause-long-covid-symptoms https://health.ucdavis.edu/news/headlines/antibodies-mimicking-the-virus-may-explain-long-haul-covid-19-rare-vaccine-side-effects/2021/11 Our previous blog in our long COVID series also explores some of the mechanisms noted above: https://www.suzannegazdamd.com/blog---long-covid/why-does-long-covid-happen Treatment approaches For both long COVID and post-vaccine injured patients, there are similar mechanisms involved. Most researchers believe that it is the lingering viral fragments (spike protein) that are wreaking havoc on the body and brain. Immune dysregulation is the common theme, and the downstream effects are discussed in our prior blog at: https://www.suzannegazdamd.com/blog---long-covid/why-does-long-covid-happen The multiplicity of mechanisms may be one reason why almost every case “is different” and why each one of these patients requires a uniquely individualized and carefully constructed protocol pertinent to their specific issues. Two different protocols but there are many more being studied around the world The treatment recommendations for LHCS are constantly evolving as we learn more about the condition. At present, we have two primary approaches that are being employed in the treatment of LHCS.
The Front Line COVID-19 Critical Care Alliance (FLCCC) provides the only published treatment protocol for vaccine-injured patients. https://covid19criticalcare.com/covid-19-protocols/i-recover-post-vaccine-treatment/ Please note their I-RECOVER Protocol is for management of long COVID patients, but there is significant overlap, and I will not review that protocol. You can find this detailed information at: https://covid19criticalcare.com/covid-19-protocols/i-recover-long-covid-treatment/ The FLCCC Recovery Protocol for Vaccine Injured Patients I encourage everyone to periodically check the content of this link for the FLCCC is updating this protocol often. https://covid19criticalcare.com/wp-content/uploads/2022/06/FLCCC_Alliance-I-RECOVER-Protocol-PostVaccine-v3-English.pdf Baseline Testing
The FLCCC protocol has first, second- and third-line approaches: First-line approach
Second-line agents
Third Line Therapy • Hyperbaric oxygen therapy (HBOT)
Other therapeutic options:
Disease Specific Therapeutic Adjuncts (Note: this section from the FLCCC is constantly being updated with new information, which we will share as available.) Small fiber neuropathy (SFN)/autonomic neuropathy
Generalized Neurologic Symptoms/Injuries/”Brain Fog”/Fatigue
Patients with an elevated DIC and those with evidence of thrombosis
Vaccine-induced myocarditis/pericarditis
Herpes virus reactivation syndrome
Tinnitus
The Patterson Protocol
Our long COVID series includes an in-depth discussion about the Patterson protocol. Dr. Bruce Patterson, formerly the Medical Director of Diagnostic Virology at Stanford University Hospitals and Clinics, California and now the founder of IncellDX, has with a team of clinicians designed a protocol that seeks to assess patient status through comprehensive lab analysis and then reduce the over-arching inflammation that can continue to cause symptoms. Dr Patterson’s research has shown that the pathophysiology behind PASC may be attributed to the recent discovery of persistent S1 protein subunit of SARS-CoV-2 in CD16+ monocytes up to 15 months after infection. CD16+ monocytes, which express both CCR5 and fractalkine receptors (CX3CR1), play a role in vascular homeostasis and endothelial immune surveillance. They believe targeting these receptors using the CCR5 antagonist, maraviroc, along with pravastatin, could disrupt the monocytic-endothelial-platelet axis that may be central to the etiology of PASC. Dr Patterson has also used components of his protocol to treat chronic Lyme disease, learn more at: https://www.suzannegazdamd.com/blog---long-covid/chronic-lyme-disease-may-have-lessons-about-long-covid Dr. Patterson’s protocol has two main goals:
With this specialized program, a specialized series of labs - the IncellKINE test - are conducted (the Incell DX panel should be used only as guidance of treatment). Based on the results, patients are then typically prescribed these therapies below; but, every patient is different and unique so the protocol is specific for each patient’s needs. Many times, we will repeat the Incell DX panel to gauge treatment response and follow clinical response as well. Now the Incell DX panel can not only measure the proinflammatory cytokines (chemical messengers) seen in Long COVID but can also quantify spike protein in monocytes and measure the monocyte subsets All of this information can be valuable in some patients with LHCS. A. Maraviroc A CCR5-antagonist, Maraviroc reduces cytokines and blocks migration of the intermediate and non-classical monocytes, as it also repolarizes the macrophages and modulates the immune system. We know that CCL5/RANTES is commonly elevated in long COVID and as an antiretroviral, Maraviroc also has been used in combination with other drugs to treat diseases including human immunodeficiency virus (HIV).
B. Statins to tamp down the CX3CR1/fractalkine pathway In order to turn off the long-term monocyte survival mechanism that’s allowing these cells to endure longer than usual. As such, statins are the second prescribed drug in the protocol. They work by inhibiting fractalkine, which stops the monocyte cells from attaching to endothelial cells on the blood vessels. Statins are shown to possess broad anti-inflammatory effects.
D. Fluvoxamine: E. Monocyte repolarization from M1 to M2 Vitamin C - 500 mg, twice a day Omega 3 - once a day Atorvastatin or Pravastatin as prescribed Melatonin – Two to 10mg at bedtime Vitamin D3/K2 - 5000 IU each day (optimum Vitamin D level is 60-100) Intravenous immunoglobulin therapy (IVIG) Expediency in treating individuals with LHCS is critical – so many patients have been suffering with numerous issues and already invested both the hours and finances in seeking help. But it is especially important to work with a clinician that understands the complexity of this problem and is committed to keeping up with the ever-changing paradigms. If we can help or answer any questions, please be sure to reach out to our offices. And be sure to stay tuned for updates - we are learning more and more every day! And remember … always be checking back with the FLCCC protocols for updates. https://covid19criticalcare.com/covid-19-protocols/ In health and hope, Dr. Suzanne K. Gazda Mazer, B. Long COVID Could Be a ‘Mass Deterioration Event’. The Atlantic. June 15, 2022. https://www.theatlantic.com/health/archive/2022/06/long-covid-chronic-illness-disability/661285/ Fox, J. Long Covid Is Showing Up in the Employment Data. Bloomberg. June 15, 2022. https://www.bloomberg.com/opinion/articles/2022-06-15/long-covid-is-showing-up-in-the-employment-data VAERS COVID data https://openvaers.com/covid-data Sisó-Almirall A, Brito-Zerón P, Conangla Ferrín L, et al. Long Covid-19: Proposed Primary Care Clinical Guidelines for Diagnosis and Disease Management. Int J Environ Res Public Health. 2021;18(8):4350. Published 2021 Apr 20. doi:10.3390/ijerph18084350 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8073248/ Proal AD and VanElzakker MB (2021) Long COVID or Post-acute Sequelae of COVID-19 (PASC): An Overview of Biological Factors That May Contribute to Persistent Symptoms. Front. Microbiol. 12:698169. doi: 10.3389/fmicb.2021.698169 https://www.frontiersin.org/articles/10.3389/fmicb.2021.698169/full#B120 FLCCC Protocol https://covid19criticalcare.com/wp-content/uploads/2021/06/FLCCC-Alliance-I-RECOVER-Management-Protocol-for-Long-Haul-COVID-19-Syndrome.pdf Lenze EJ, Mattar C, Zorumski CF, et al. Fluvoxamine vs Placebo and Clinical Deterioration in Outpatients With Symptomatic COVID-19: A Randomized Clinical Trial. JAMA. 2020;324(22):2292–2300. doi:10.1001/jama.2020.22760 https://jamanetwork.com/journals/jama/fullarticle/2773108#jpc200006r26 Glebov OO (2021) Low-Dose Fluvoxamine Modulates Endocytic Trafficking of SARS-CoV-2 Spike Protein: A Potential Mechanism for Anti-COVID-19 Protection by Antidepressants. Front. Pharmacol. 12:787261. doi: 10.3389/fphar.2021.787261 https://www.frontiersin.org/articles/10.3389/fphar.2021.787261/full Hyperbaric oxygen therapy for the treatment of long COVID: early evaluation of a highly promising intervention. https://react19.org/wp-content/uploads/2022/05/33439.pdf Vedicinals https://www.vedicinals.com/vedicinals-9/ Lehrer S, Rheinstein PH. Ivermectin Docks to the SARS-CoV-2 Spike Receptor-binding Domain Attached to ACE2. In Vivo. 2020;34(5):3023-3026. doi:10.21873/invivo.12134 https://pubmed.ncbi.nlm.nih.gov/32871846/ Zhang X, Song Y, Ci X, et al. Ivermectin inhibits LPS-induced production of inflammatory cytokines and improves LPS-induced survival in mice. Inflamm Res. 2008;57(11):524-529. doi:10.1007/s00011-008-8007-8; https://pubmed.ncbi.nlm.nih.gov/19109745/ Lipopolysaccharide-Induced Inflammation. https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/lipopolysaccharide-induced-inflammation Patterson BK, Francisco EB, Yogendra R, et al. Persistence of SARS-CoV2-2 S1 Protein in CD16+ Monocytes in Post-Acute Sequelae of Covid-19 (PASC) up to 15 months post-infection. Front Immunol. 2022 Patterson BK, Seethamraju H, Dhody K, et al. CCR5 Inhibition in Critical COVID-19 Patients Decreases Inflammatory Cytokines, Increases CD8 T-cells, and Decreases SARS-CoV2 RNA in Plasma by Day 14. International Journal of Infectious Diseases. 2021; 103:25-32. Short-Term Treatment With Atorvastatin Reduces Platelet CD40 Ligand and Thrombin Generation in Hypercholesterolemic Patients Circulation Feb 2005 https://www.ahajournals.org/doi/10.1161/01.cir.0000153810.81187.7d#:~:text=Compared%20with%20diet%2Dassigned%20patients,of%20its%20cholesterol%2Dlowering%20effect Patterson, BK., Yogendera, R., et al. Targeting the Monocytic-Endothelial-Platelet Axis with Maraviroc and Pravastatin as a Therapeutic Option to Treat Long COVID/ Post-Acute Sequelae of COVID (PASC). ResearchGate. (February 2022) http://dx.doi.org/10.21203/rs.3.rs-1344323/v1
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorSuzanne Gazda M.D. Neurologist Archives
January 2024
Categories |








 RSS Feed
RSS Feed