|
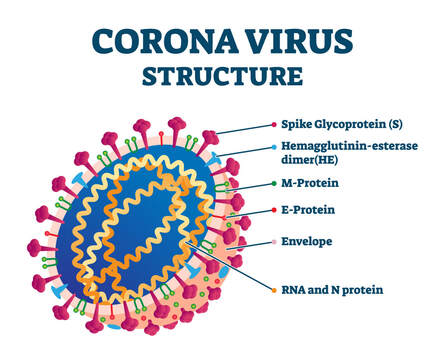
Autoimmunity occurs when immune system activity, primarily inflammation, is directed at healthy cells, tissues, or other inappropriate targets in the body. It seems that COVID-19 shares a similar inflammatory immune response with auto-inflammatory and autoimmune conditions. And given that some may say we were already in the midst of what could be considered an “autoimmune epidemic” tied to numerous neurological and systemic diseases, this just adds to the daunting situation we face now and in the future. In a recent study in the Journal of Immunology, evidence shows that SARS-CoV-2 may cause the body’s immune system to mistakenly attack its own cells and tissues — in the heart, in the brain, the lungs and elsewhere because there are a number of similarities between the amino acid sequences of coronavirus proteins and those of human proteins In this mechanism, antibodies formed against SARS-CoV-2 would also bind to human tissue proteins leading to autoimmune reactivity. There also has been research that sheds more light on these mechanisms. In a 2021 published paper, “Reaction of Human Monoclonal Antibodies to SARS-CoV-2 Proteins with Tissue Antigens: Implications for Autoimmune Diseases”, the authors “sought to determine whether immune reactivity occurs between anti-SARS-CoV-2 protein antibodies and human tissue antigens, and whether molecular mimicry between COVID-19 viral proteins and human tissues could be the cause.”1 They identified significant cross-reactivity between SARS-CoV-2 proteins (spike protein, nucleoprotein, envelope protein, and membrane protein) with 55 different human tissues using monoclonal and polyclonal antibodies and performed epitope mapping to identify the relationships. These findings could shed light on the multi-systemic diseases that manifest in some patients with COVID-19. It also partially explains why a subset of susceptible individuals may develop multi-system reactions due to autoimmune cross-reactivity and why some people with these infections may develop autoimmunity post-COVID due to these very same relationships. At what point in the study was molecular mimicry at its highest? And what is affected? The mitochondria showed the most cross reactivity with the spike protein and nucleoprotein were highly correlated to mitochondria. This, plus the tremendous amount of ongoing oxidative stress with a viral illness, is a recipe for chronic fatigue and many other downstream effects:
The big questions: will we see a rise in autoimmune and neurodegenerative disease, post-COVID or post-vaccine? Post-vaccine or viral-induced autoimmunity is not a new topic. The COVID vaccine is comprised of mRNA delivered to cells, which then cause the production of the SARS-CoV-2 spike protein. So at this time we simply do not have all the information available to know if the vaccine may lead to long term side effects simply as a result of its own mechanisms. Additionally there is a concern that with vaccine administration when some people are exposed to the virus, more serious disease may occur through antibody-dependent immune enhancement or pathogen priming that triggers an autoimmune response. It sometimes can take anywhere from 3-12 years for the immune system to manifest an outcome from the dysregulated immune response in the form of an autoimmune disease. As indicated in one study’s conclusions “Because of the cross-reactivity of the SARS- CoV-2 proteins with human tissues and the possibility of either inducing autoimmunity, exacerbating already unhealthy conditions, or otherwise resulting in unforeseen consequences, it would only be prudent to do more extensive research regarding the autoimmune-inducing capacity of the SARS-CoV-2 antigens and as well the COVID vaccine. An insufficiently vetted vaccine might mean trading freedom from COVID-19 to an autoimmune assault in the future." It’s important to note that only a subset of individuals with COVID-19 infections will express into autoimmunity due to many factors beyond just cross-reactivity, including gene susceptibility and immune tolerance individuality. But given the number of patients who have had COVID 19, this could still be a substantially large number in the future. More about mRNA All mRNA vaccines effect the coded protein production in the recipient’s body. In the case of COVID-19, inert spike (S) antigen proteins are produced. Normally, these enable SARS-CoV-2 coronavirus particles to enter host cells, but therapeutically, inoculation triggers humoral (antibody-mediated) acquired immunity. Researchers studied the relationships between spike and nuclear proteins of SARS-CoV-2 and autoimmune target proteins and noted:
The question too is whether when we genetically engineer the cells to produce the SARS-CoV-2 spike protein, will they always be creating this protein and an antibody response? We know from these cited studies that the spike protein can induce molecular mimicry and tissue damage. The vaccine only attenuates, vs. prevents, COVID. So it’s imperative to learn more about its efficacy and both short and long-term actions as well as the safety of any treatment for the virus itself. Now is the time to live an anti-inflammatory life! Given the sheer timing of these events, there are many things we just don’t yet know although the scientific community is continuing to study this rapidly changing situation to better understand all implications. However, our world clearly should not have needed COVID 19 or another viral outbreak to serve as a wake-up call to understand that we must – and can - modify our risk of inflammation and subsequent disease initiation. We really do have the ability right now to strengthen our immune health through a healthy diet, to improve our gut health, make lifestyle modifications that support optimum wellness, and take the appropriate measures to reduce our potential for systemic inflammation. Autoimmune and neuroimmune diseases were already here. And without seriously rethinking things like bad diets, toxic environmental or other triggers and more, are we just setting the stage for additional chronic diagnoses that constitute another global health crisis? More than ever before, applying sound principles of health is our brain and our body’s best defense to fight inflammation, infection and ideally achieve a state of wellbeing that, quite simply, affords us a better quality of life. In hope and healing, Suzanne K Gazda MD References: 1 Vojdani A, Vojdani E and Kharrazian D (2021) Reaction of Human Monoclonal Antibodies to SARS-CoV-2 Proteins With Tissue Antigens: Implications for Autoimmune Diseases. Front. Immunol. 11:617089. doi: 10.3389/fimmu.2020.617089 https://www.frontiersin.org/articles/10.3389/fimmu.2020.617089/full?fbclid=IwAR2omo1nx2CfIaV2wXondJdDzwwVbN3g2D7LOUfJC-t4oPAo_D3hNHpS1S4 2 Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5(11):1265–1273. doi:10.1001/jamacardio.2020.3557 3 Doshi Peter. Will covid-19 vaccines save lives? Current trials aren’t designed to tell us BMJ 2020; 371 :m4037 Additional reading: Arvin AM, Fink K, Schmid MA, Cathcart A, Spreafico R, Havenar-Daughton C, Lanzavecchia A, Corti D, Virgin HW. A perspective on potential antibody-dependent enhancement of SARS-CoV-2. Nature. 2020 Aug;584(7821):353-363. doi: 10.1038/s41586- 020-2538-8. Epub 2020 Jul 13. PMID: 32659783. https://www.nature.com/articles/s41586-020-2538-8 https://www.suzannegazdamd.com/blog/it-shouldnt-take-a-pandemic-for-us-to-take-a-long-look-at-our-health-trends https://www.suzannegazdamd.com/blog/is-there-more-to-immune-mediated-dysfunction-in-even-more-neurological-disorders The Autoimmune Epidemic by Donna Jackson Nakazawa https://www.amazon.com/Autoimmune-Epidemic-Donna-Jackson-Nakazawa/dp/0743277767
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorDr. Suzanne Gazda, Integrative Neurology Archives
February 2024
Categories |

 RSS Feed
RSS Feed