|
In my last blog, I covered in great detail the complex mechanisms that in many long hauler COVID patients can cause a number of neurological issues, including headaches. We know that headaches especially for some individuals (e.g. migraine sufferers) can be extremely debilitating, even when experienced on an occasional basis. And with long COVID, and regardless of the relative mildness or severity of an original infection, these headaches can be daily and feel almost never ending. Our practice is working with more and more patients in recent months and providing several therapeutic measures to address both the symptoms and root cause of what starts as inflammation and left unchecked may indeed spiral into more problems. Treatment Strategies Our practice is working with more and more patients in recent months and providing several therapeutic measures to address both the symptoms and root cause of what starts as inflammation and left unchecked may indeed spiral into more problems. An approach to improving headache symptoms in long COVID may include, as appropriate to each patient’s condition:
Target treatment to type of headache. 1. Migraine severe unilateral/throbbing worsens with movement and associated with either nausea and/or vomiting or light or sound sensitivity. Some migraines are preceded by an aura, which may include visual disturbances or sensations such as flashing lights or zigzag lines. 2. Migraine with aura: may include at least one of the following, but with no motor weakness: • Fully reversible dysphasic speech disturbance where speech is temporarily disrupted. • Sensory symptoms that are fully reversible, including positive features (e.g., pins and needles) and/or negative features (e.g., numbness). • Visual symptoms that are fully reversible, including positive features (e.g., flickering lights, spots, lines) and/or negative features (e.g., loss of vision) 3. Tension headache: mild to moderate, bilateral, pressure-like, not aggravated by movement and should not be associated with light/sound sensitivity and nausea. • For prevention we use Amitriptyline 25-75mg hs , Nortriptyline 25-75mg hs , Protriptyline 20-30mg given in the a.m. for it is activating, or Effexor 150mg. Acute migraines. There are a number of approaches to treating migraine headaches: --First-line agents: NSAIDS or combination analgesics such as Excedrin (aspirin + acetaminophen + caffeine) Also Triptans, Diclofenac --Second line: Celebrex, Relafen, and Mobic with prochloperazine 10 mg, three times daily, or every night at bedtime for three days, or Promethazine 25-50 mg --Migraine-specific agents: If the headaches don’t respond to first-line agents, try one of these: Triptans:
The best results occur when triptans are taken early in an attack. For migraine with aura, evidence suggests that the best results are achieved by taking the triptan early in an attack, at the onset of pain rather than the onset of aura; however, taking a triptan during a typical aura also appears to be safe. Triptans are generally well tolerated. A 2016 meta-analysis found no significantly increased risk of serious adverse effects.2 Commonly experienced side effects of triptans can include:
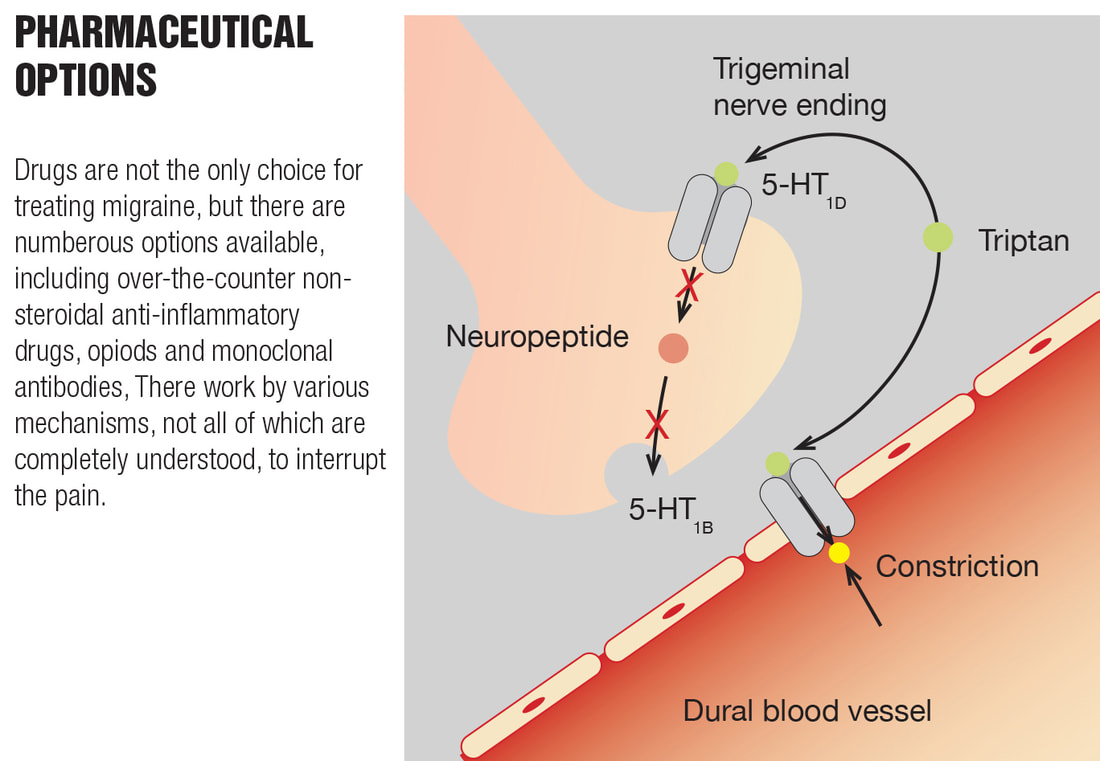
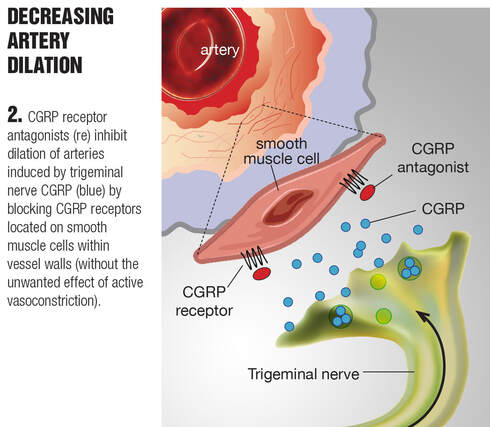
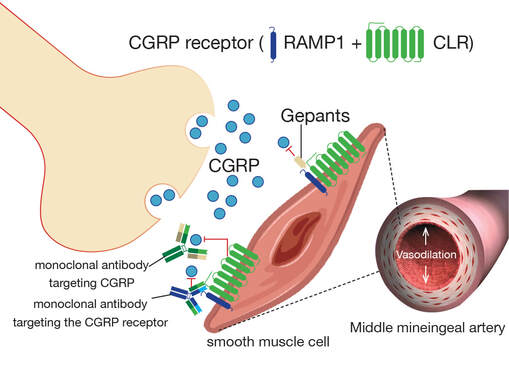
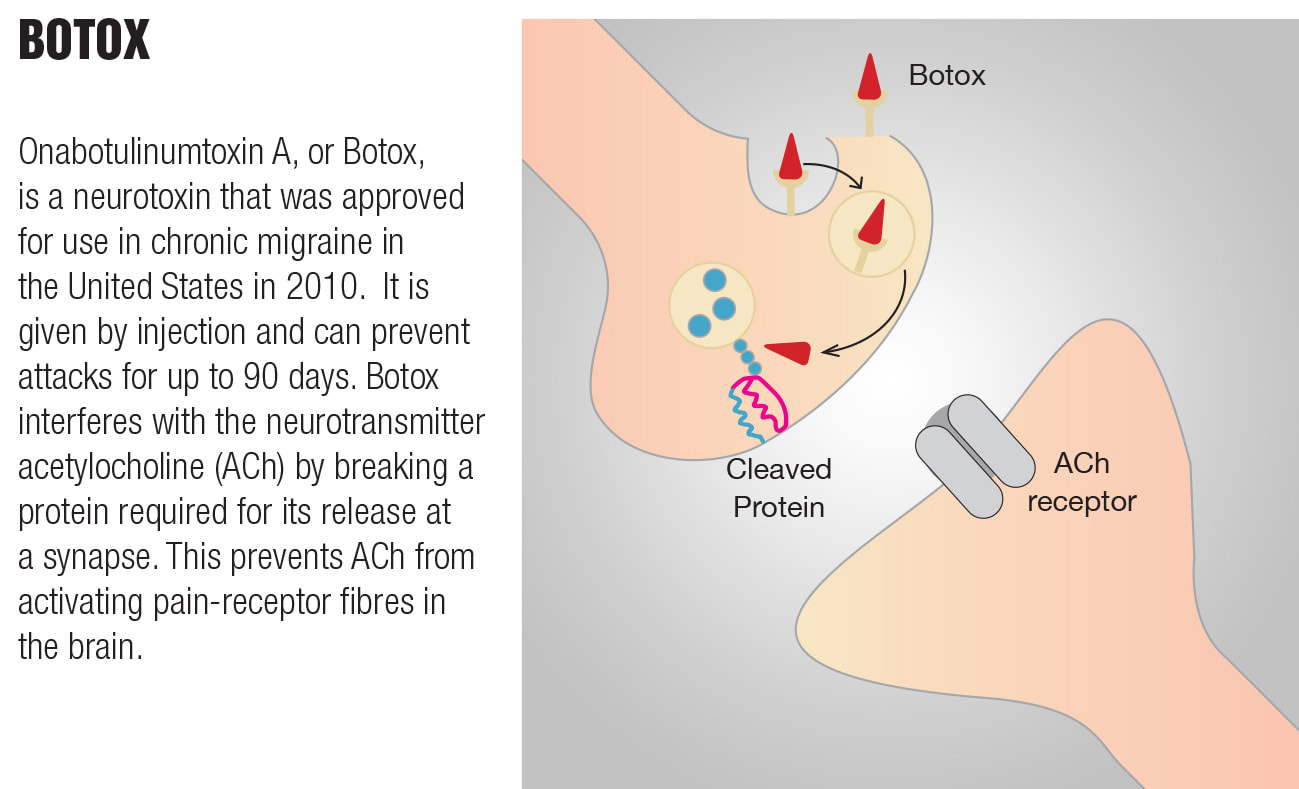
Some people may also experience a generalized feeling of being sick, dry mouth, and drowsiness. All triptans should be limited to no more than 10 days of use per month to avoid medication overuse headache. Based on limited evidence, it is still recommended that triptans be avoided in patients with peripheral vascular disease, hemiplegic migraine, basilar migraine, ischemic stroke, ischemic heart disease, Prinzmetal's angina, uncontrolled hypertension, ischemic bowel disease, cerebrovascular syndromes, and in those who are pregnant.3 They mimic the activity of the neurotransmitter serotonin (5-HT) and are effective in the early stages of an attack. At 5-HT1B receptors, they reduce pain by causing cranial blood vessels to constrict. At 5-HT1D receptors, they block the release of neuropeptides that trigger inflammation. Almotripta Almotriptan (Axert) 6.25-12.5mg as single dose No more than 25 mg in 24 hours Eletriptan (Relpax) 20- and 40-mg tablets - Least cardiovascular risk Frovatriptan (Frova) 2.5 mg - Recommended for menstrual migraine Naratriptan (Amerge) 1 and 2.5 mg Rizatriptan (Maxalt) 5 and 10 mg tablet and also orally disintegrating tab Sumatriptan (Imitrex) 25, 50, 100 mg 6 mg injection 5 or 20 mg nasal spray Oral and intranasal formulations, and subcutaneous injection Zolmitriptan (Zomig) 2.5 or 5 mg tab and orally disintegrating tablets and 5 mg nasal spray Sumatriptan/naproxen 85/500mg (Treximet) Take at onset of headache. May repeat in 2 hours No more than 2 tablets in 24 hours Naratriptan and frovatriptan have the slowest onset of action among the triptans and may have the lowest propensity to cause side effects. Combination with monoamine oxidase inhibitors is relatively contraindicated with triptans because of the risk of serotonin syndrome. Triptans should not be used within 24 hours of the use of ergotamine preparations or a different triptan medication as serotonin syndrome is a concern.4 The drug eletriptan is primarily metabolized by cytochrome P-450 enzyme CYP3A4. Therefore, eletriptan should not be used within at least 72 hours of treatment with other drugs that are potent CYP3A4 inhibitors, such as ketoconazole, itraconazole, nefazodone, troleandomycin, clarithromycin, ritonavir, and nelfinavir. The dose of rizatriptan must be reduced to 5 mg in patients taking propranolol. For more information regarding these and other prescribed medications for the treatment of migraine, you can read more at: https://www.webmd.com/migraines-headaches/migraine-treatments https://www.rxlist.com/migraine_medications/drugs-condition.htm https://www.healthline.com/health/migraine-drugs#triptans What other options are there? In the event that triptans have not helped or there is a contraindication for use, gepants may be employed. Note: in most instances, a patient has to have failed triptans or be unable to take this class of medication in order to obtain insurance coverage for a gepant prescription. Gepants are small molecule calcitonin gene-related peptide (CGRP) receptor antagonists. Calcitonin gene-related peptide (CGRP) is a protein that carries pain signals along nerves that are involved in generating the headache pain associated with migraine. Gepants work to block CGRP from attaching to its receptor and initiating those pain signals; they do not cause vasoconstriction per se.5 The drugs are available in two forms - small molecules called gepants (Nurtec, Ubrelvy, and Qulipta) and large molecule monoclonal antibodies (Aimovig, Ajovy, Emgality, and Vyepti). Both forms disrupt CGRP action by preventing it from binding to and activating its receptor, and therefore, the migraine chain reaction is thwarted. Learn more about the action of CGRP at: https://www.suzannegazdamd.com/blog/migraines-the-science-causes-and-treatment-options Rimegepant (Nurtec ODT): The maximum dosage of rimegepant is a single 75 mg dose as needed per 24 hour treatment; rimegepant does not appear to be associated with medication-overuse headache. Ubrogepant: Recommended 50-100 mg for acute migraine and, if needed, patients may take second dose at least 2 hours after initial dose, with a maximum dose of 200 mg/day. Note: There are many potential drug interactions with this class of medications. Be sure and check with your doctor or pharmacist Additional options: ditans Ditans are a class of “abortive” medications for the treatment of migraines, which selectively bind to the 5-HT1F receptor subtype. Lasmidtitan (Reyvow): This drug is a serotonin 5-HT1F receptor agonists. Ditans do not elicit a vasoconstrictive effect, whereas triptans cause vasoconstriction via agonistic action at 5-HT1B/1D receptors.5 It has better two-hour pain results, but the side effects are dizziness and sedation so patients cannot drive for at least eight (8) hours. It is a schedule 5 drug; dose for adults is 50 mg, 100 mg, or 200 mg per day as needed. Patients should not take more than one dose within a 24-hour period. Additionally, ergotamine (nasal spray) may be helpful. Ergotamine is an ergot alkaloid medicine that is used to treat or prevent a vascular headache (such as a migraine or cluster headache). It is not intended for daily use and will not treat headache pain. As needed, anti-nausea medications (antiemetics) such as Zofran, Phenergan, or Compazine and their generic formularies also may be prescribed for associated symptoms. Migraine Preventative Therapies. These medications are appropriate for a patient experiencing more than two migraines a week, with the understanding that prophylactic medication won’t prevent all headaches. At best, medication alone can be expected to cut the number of headaches in half.
Learn more about why long COVID occurs at: https://www.suzannegazdamd.com/blog---long-covid/why-does-long-covid-happen Note: For insurers to approve a CGRP inhibitor:
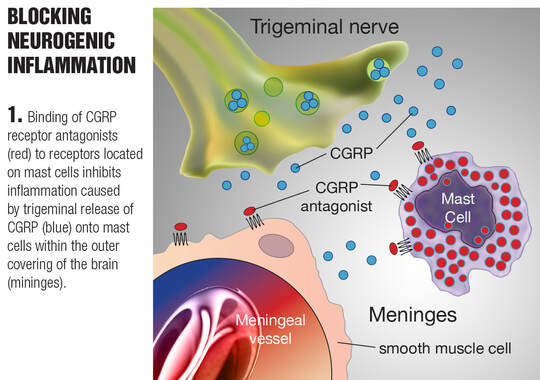
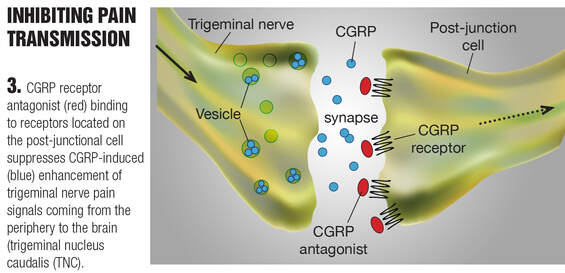
How do CGRP inhibitors work? The pathophysiology of migraine is understood to develop from a cascade of events within the nervous system and vasculature (blood vessels) of the brain, with calcitonin gene-related peptide (CGRP) being one player in a large cast. Initial depolarization of central nervous system neurons (nerve cells) spreads and triggers trigeminal nerve fibers, resulting in pain. The trigeminal nerve network releases CGRP, among other proteins that mediate inflammation and vascular tone. CGRP is active in pain signal transmission, vasodilator effects (blood vessel dilation), and brain inflammation, all of which amplify the headache pain. Blocking CGRP can interrupt the sequence of migraine mechanisms and thereby provide relief from an attack or prevention when used regularly. Anti-CGRP agents work by either binding to CGRP itself or to the CGRP receptor site. An overview of some anti migraine drugs that directly block CGRP or its receptor. Since CGRP plays an important role in the pathophysiology of migraine, in the last few decades new anti migraine drugs have been developed for migraine treatment. These drugs include (i) gepants, which act by directly blocking the CGRP receptor (i.e. rmiegepant and atogepant); and (ii) monoclonal antibodies, which directly block CGRP (i.e.eptinezumab, fremanezumab and galcanezumab or its receptor (i.e. erenumab). CLR, calcitonin receptor-like receptor; RA<P1, receptor activity-modifying protein 1.
Complementary therapies in addition to prescribed medications may include:
Additional drug therapies to consider:
Indomethacin for refractory COVID headache: After treatment with indomethacin, 36 patients reported greater than 50% headache relief from the third day and 5 patients became asymptomatic on the fifth day.6 In addition to the inhibition of cyclooxygenase, preventing the production of prostaglandins from arachidonic acid, indomethacin has a unique action that is not yet clarified. It may interfere with iontophoresed glutamate-activated dural-responsive second order neurons in the Trigeminal Nucleus Caudalis. Moreover, indomethacin may modulate nitric oxide (NO) signaling pathways. Nitric oxide is known to induce headache and delayed migraine in patients. In some cases, indomethacin therapy caused persistent inhibition of platelet function. Patients suffering from classic migraine showed a high incidence of platelet activation (>90%) in comparison with common migraine patients. For patients whose individual health condition may preclude use of some of these other or newer pharmaceutical options, there are studies that point to relief using: • Fluvoxamine In one study compared to the tricyclic antidepressant amitriptyline, fluvoxamine showed better migraine reduction and less drowsy side effects7; additionally, selective serotonin reuptake inhibitors (SSRIs) like fluvoxamine inhibit mast cell activation.8 https://www.jimmunol.org/content/202/1_Supplement/54.11 • Ibuprofen (Advil, Motrin) The non-steroidal anti-inflammatory agent, ibuprofen, also has been implicated in raising ACE2 levels. In a study of rats with type 1 diabetes, ibuprofen raised cardiac ACE2 protein levels, or more correctly, attenuated the diabetes-induced reduction in ACE2 levels.9 Qiao W, Wang C, Chen B, et al. Ibuprofen attenuates cardiac fibrosis in streptozotocin-induced diabetic rats. Cardiology. 2015;131(2):97–106. [Crossref], Devices for migraine treatment. While costly, there are a number of devices may be preferred by people who want to avoid medication side effects: https://www.goodrx.com/conditions/migraine/consumer-devices-for-migraine-treatment-and-prevention In summary, we know that there are many treatment options for headaches. And as we continue to see more instances of headaches in our long COVID patients, we must keep in mind the mechanisms driving these symptoms, including high levels of systemic and brain inflammation as well the propensity for thrombosis generated by spike protein. Addressing this inflammation, much like we do with all neurological autoimmune disease, is key to achieving more successful outcomes. In our practice, we are utilizing a comprehensive long hauler recovery protocol designed to treat headaches as well as numerous other symptoms in order to ultimately help heal the whole patient. There is no single therapeutic protocol with efficacy for all patients, so it is imperative to consult a clinician with experience in treating long-haulers syndrome. Please continue to check back for additional articles in our long COVID series and don’t hesitate to reach out to our offices if we can help or if you’d like to schedule a visit. In hope and health, Dr. Suzanne Gazda Reference 1 George, J. Migraine Frequency, Severity Drop Substantially With Diet Interventions. MedPage Today. July 2021. https://www.medpagetoday.com/neurology/migraines/93375 See also: BMJ 2021;374:n1535; https://www.bmj.com/content/374/bmj.n1535 2 Mayans, L., Walling, A. Acute Migraine Headache: Treatment Strategies. Am Fam Physician. 2018;97(4):243-251.https://www.aafp.org/pubs/afp/issues/2018/0215/p243.html#afp20180215p243-b27 3 Jamieson DG. The safety of triptans in the treatment of patients with migraine. Am J Med. 2002 Feb 1;112(2):135-40. doi: 10.1016/s0002-9343(01)01064-6. PMID: 11835952. 4 Gillman PK. Triptans, serotonin agonists, and serotonin syndrome (serotonin toxicity): a review. Headache. 2010;50(2):264-272. doi:10.1111/j.1526-4610.2009.01575.x 5 Edvinsson L. CGRP receptor antagonists and antibodies against CGRP and its receptor in migraine treatment. Br J Clin Pharmacol. 2015;80(2):193-199. doi:10.1111/bcp.12618 6 Krymchantowski AV, Silva-Néto RP, Jevoux C, Krymchantowski AG. Indomethacin for refractory COVID or post-COVID headache: a retrospective study. Acta Neurol Belg. 2022;122(2):465-469. doi:10.1007/s13760-021-01790-3 7 Bánk J. A comparative study of amitriptyline and fluvoxamine in migraine prophylaxis. Headache. 1994;34(8):476-478. doi:10.1111/j.1526-4610.1994.hed3408476.x 8 Selective Serotonin Reuptake Inhibitors Suppress Mast Cell Function Haque, T., Ryan, J. Selective Serotonin Reuptake Inhibitors Suppress Mast Cell Function. The Journal of Immunology, May 1, 2019, 202 (1 Supplement) 54.11; https://www.jimmunol.org/content/202/1_Supplement/54.11 9 Saghir Akhtar, Ibrahim F. Benter, Mohammed I. Danjuma, Suhail A. R. Doi, Syed S. Hasan & Abdella M. Habib (2020) Pharmacotherapy in COVID-19 patients: a review of ACE2-raising drugs and their clinical safety, Journal of Drug Targeting, 28:7-8, 683-699, DOI: 10.1080/1061186X.2020.1797754 Additional reading: Acute migraine treatment https://www.uptodate.com/contents/acute-treatment-of-migraine-in-adults/abstract/79 See also: https://www.aafp.org/pubs/afp/issues/2018/0215/p243.html#afp20180215p243-b12 Migraine treatments https://www.webmd.com/migraines-headaches/migraine-treatments The American Headache Society Consensus Statement: Update on integrating new migraine treatments into clinical practice https://headachejournal.onlinelibrary.wiley.com/doi/10.1111/head.14153 CGRP inhibitors for migraine prophylaxis: a safety review https://www.tandfonline.com/doi/pdf/10.1080/14740338.2020.1811229 The efficacy and safety of venlafaxine in the prophylaxis of migraine https://pubmed.ncbi.nlm.nih.gov/15705120/ A randomized trial of divalproex sodium extended-release tablets in migraine prophylaxis https://n.neurology.org/content/58/11/1652
6 Comments
1/18/2023 01:47:45 am
Researchers who research on the human brain and psychology say that around one in six people around the world have a headache, half of them have a migraine, that is, a headache. For getting more details about "cause of headaches" then click on given link.
Reply
6/19/2023 04:31:27 am
After reading this article, I found the information about how Botox works to be particularly interesting. By doing Botox treatment, it effectively prevents the activation of pain networks in the brain. This mechanism of action sounds promising and could potentially provide much-needed relief for chronic headache sufferers. Thank you for sharing this informative piece!
Reply
Reply
1/22/2024 12:41:30 pm
The Chrome Hearts line of clothes for women, which comes in many colors and styles, is a great way for them to show off their style. On the other hand, our range of clothes for men makes them stand out. We now have t-shirts, hoodies, jackets, and pants for both men and women, as well as a Sp5der hoodie for guys. You can wear these things on casual days or whenever you want to spice up your boring daily life. We've been working hard to make trendy, colorful, and easy-to-wear clothes that are one-of-a-kind. We've worked together with hundreds of customers on hundreds of projects after they made a request
Reply
1/22/2024 12:44:33 pm
This streetwear brand was founded by Young Thug, a rapper known for his bold style. Fans and fashion crowds will get a taste of his eccentric style. A pioneer of streetwear, Sp5der has revolutionized streetwear with its unique colors and spider web motifs on the shoulders of denim trucker jackets. There are also items in the Spider collection that feature the spider web motif, such as t-shirts and caps, which feature spider webs of various sizes and shapes.
Reply
James
1/24/2024 04:23:36 am
Reply
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorSuzanne Gazda M.D. Neurologist Archives
January 2024
Categories |

 RSS Feed
RSS Feed