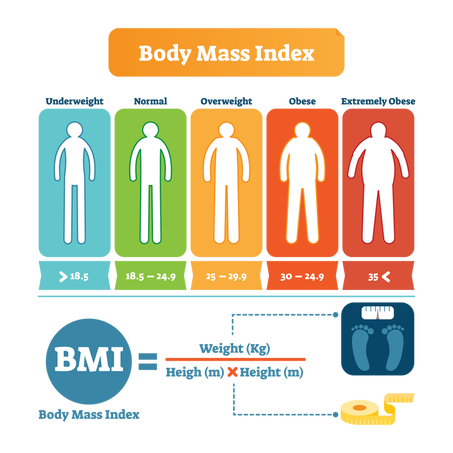
And studies that specifically looked at the incidence of MS in obese children show trends that have truly alarming implications about the wellbeing of our future generation. Findings based upon years of extensive research have examined the relationship between obesity and the onset and progression of neurological diseases such as Parkinson’s and Alzheimer’s as well.1 And now, the epidemic of obesity has converged with the current pandemic, providing additional evidence that people with obesity are at a greater risk of severe disease and death due to COVID-19.2 In this study, researchers show how obesity dysregulates the immune system where both innate and adaptive immune response are impaired and individuals with obesity are in a state of chronic and low-grade inflammation. Article authors noted that “data over the years have indicated that obesity negatively impacts host immune defense, making it vulnerable to infectious disease. Excess adiposity is associated with significant changes in the resident immune cell composition of adipose tissue, which disrupts the balance between pro-inflammatory and anti-inflammatory immune cells in favor of the former. This leads to a state of chronic low-grade inflammation. This chronic inflammation is likely amplified by acute inflammation arising out of COVID-19 resulting in a more severe disease phenotype and poorer outcomes.” It’s not as if we as a society were unaware of these indicators. “Influenza and obesity: its odd relationship and the lessons for COVID-19 pandemic” took a close look at the link between obesity and influenza, for example, and the parallels to today’s pandemic are striking. Some findings included that a “defective response of both innate and adaptive immune system and sedentariness are major determinants in the severity of influenza viral infection in obese patients.” The article also stated that being overweight not only increases the risk of infection and of complications for the single obese person, but a large prevalence of obese individuals within the population might increase the chance of appearance of more virulent viral strain.3 This is indeed sobering news as so many Americans are unfortunately struggling even more now with being overweight. Our brain and obesity. Earlier this year, researchers published a study that found a link between obesity around the stomach area and smaller brain size - specifically, lower gray matter volume. As discussed in an article in Medical News Today, the findings of another recent study showed that the brain’s prefrontal cortex, which is a critical area for complex thinking, planning, and self-control, is less active in people who tend to overeat and this in turn may lead to obesity and weight gain. In the journal Radiology, the work of Dr. Ilona A. Dekkers’, Leiden University Medical Center in the Netherlands, detailed the results of a team of researchers using advanced MRI scanning technology to understand the link between obesity and brain structure.4 Dr. Dekkers and team reported smaller gray matter volumes in people with obesity and noted that “having higher levels of fat distributed over the body is associated with smaller volumes of important structures of the brain, including gray matter structures that are located in the center of the brain.” This was a major study where they examined brain scans from over 12,000 people who took part in the United Kingdom Biobank Imaging study. An extensive brain imaging study published in 2020 in the Journal of Alzheimer’s Disease highlighted even more frightening data, citing that “as a person's weight goes up, all regions of the brain go down in activity and blood flow.” Analyzing over 35,000 functional neuroimaging scans using single-photon emission computerized tomography (SPECT) from more than 17,000 individuals to measure blood flow and brain activity, the study showed that being overweight or obese seriously affects brain activity as it also increases the risk for Alzheimer's disease and other psychiatric and cognitive conditions. From poor nutritional choices to sedentary lifestyles, 2020 didn’t help at all. In January of just this year, a new study found that a brain pressure disorder called idiopathic intracranial hypertension is on the rise, especially in socioeconomically vulnerable populations, and the increase corresponds with rising obesity rates and a high body mass index (BMI).5 According to the World Health Organization (WHO), a BMI of at least 30 kg/m2 is considered obese, between 25 and 30 is considered overweight, between 18.5 and 25 is considered healthy weight, and below 18.5 is considered underweight. Current statistics in this country based on the latest data from the Centers for Disease Control and Prevention (CDC) indicate that the prevalence of obesity was 42.4%, the first time the figure has crossed the 42% threshold. But 71.6% of all American adults age 20 and above were overweight. We can only assume these figures will look even worse after so many people faced economic and lifestyle challenges during the last year that may have affected their ability to obtain nutritious foods. The risk factors that lead to chronic neuroinflammation are vast and obesity, albeit a major factor, is just one. Lack of exercise, poor dietary choices (the Standard American Diet), hypertension, gut dysbiosis, smoking, excessive alcohol intake and high levels of stress all contribute to the likelihood of severe COVID disease and poor outcomes.
So what we can do? Talk to your doctor before beginning any exercise program or making dramatic dietary changes – you don’t want to exchange one problem for another, but the idea is to start with attainable goals. Stop smoking (your heart will thank you too), reduce your sugar consumption, swap whole foods for processed, and cut back on high sodium snacks. If you are struggling with your weight, you may find seated exercise a more viable option; check out these suggestions from VeryWell Fit: https://www.verywellfit.com/seated-total-body-for-overweight-and-obese-exercisers-1231355 https://www.verywellfit.com/best-workouts-if-youre-overweight-3495993 Patients who are obese didn’t become that way overnight and this pandemic only exacerbated a trend that existed pre-COVID. So remember this is not something you can instantly resolve overnight either. But you may be surprised at how giving up sugary soda means having increased energy and clarity of mind. Or that stepping outside for a short walk around the block and getting some valuable sunlight can boost your spirits and your motivation. If possible, get your family involved too and improve your odds of committing to improved health potential. Change is always easier with a support system so enlist your loved ones (their brain and overall health can benefit too) and don’t hesitate to talk to your family physician or a nutritionist for even more help. In hope and healing, Dr. Suzanne Gazda You’ll find additional dietary-related information here as well as on our website – just use the Search bar function located on each page and type in a key word or two to read more articles: https://www.suzannegazdamd.com/uploads/3/8/3/4/38341157/nutritional_approaches_in_ms.pdf https://www.suzannegazdamd.com/scientifically-speaking1/the-importance-of-the-microbiome-in-multiple-sclerosis https://www.suzannegazdamd.com/blog/new-study-shows-lower-risk-of-ms-relapse-with-the-prudent-diet https://www.suzannegazdamd.com/blog/why-is-nutrition-so-important-in-pans-and-pandas https://www.suzannegazdamd.com/blog/it-shouldnt-take-a-pandemic-for-us-to-take-a-long-look-at-our-health-trends References: 1 Bhat, Z. F., Morton, J. D., Mason, S., Bekhit, A., & Bhat, H. F. (2019). Obesity and neurological disorders: Dietary perspective of a global menace. Critical reviews in food science and nutrition, 59(8), 1294–1310. https://doi.org/10.1080/10408398.2017.1404442 2 Mohammad, S., Aziz, R., Al Mahri, S. et al. Obesity and COVID-19: what makes obese host so vulnerable?. Immun Ageing 18, 1 (2021). https://doi.org/10.1186/s12979-020-00212-x 3 Luzi, L., & Radaelli, M. G. (2020). Influenza and obesity: its odd relationship and the lessons for COVID-19 pandemic. Acta diabetologica, 57(6), 759–764. https://doi.org/10.1007/s00592-020-01522-8 4 Sandalou, A. Obesity and the 'self-control' brain area: What is the link? Medical News Today (2019) https://www.medicalnewstoday.com/articles/324560#The-role-of-the-prefrontal-cortex-in-obesity 5 Latif Miah, Huw Strafford, Beata Fonferko-Shadrach, Joe Hollinghurst, Inder MS Sawhney, Savvas Hadjikoutis, Mark I Rees, Rob Powell, Arron Lacey, W Owen Pickrell. Incidence, Prevalence and Healthcare Outcomes in Idiopathic Intracranial Hypertension: A Population Study. Neurology (January 2021). https://n.neurology.org/content/early/2021/01/20/WNL.0000000000011463
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorDr. Suzanne Gazda, Integrative Neurology Archives
February 2024
Categories |
 RSS Feed
RSS Feed