|
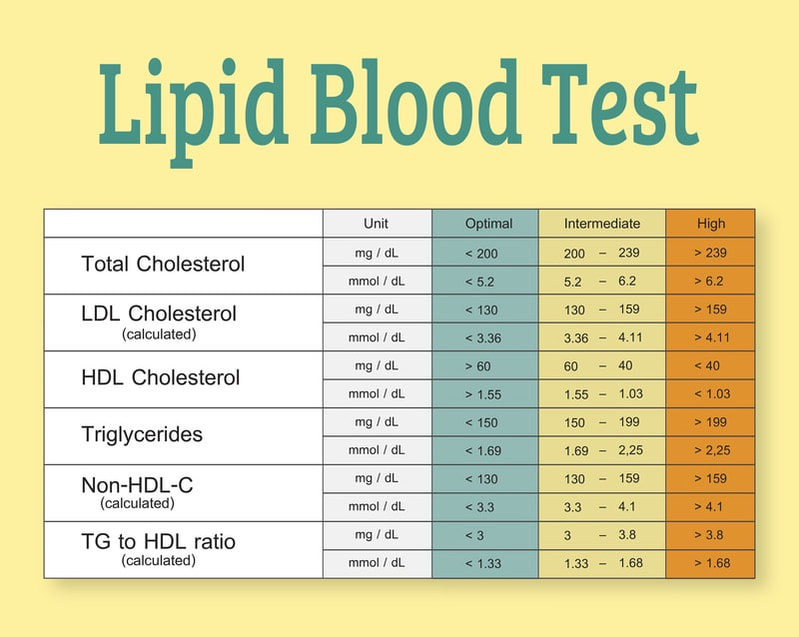
I believe the role of high or abnormal lipid ratios in the body and the brain is tied to INFLAMMATION and, as with any disease, we know that inflammation fuels the fire. Lipid markers are well established predictors of vascular disease. The most frequently measured lipid variables are total cholesterol (TC), high density lipoprotein cholesterol (HDL), low density lipoprotein cholesterol (LDL) and triglycerides (TG). Abnormal lipid markers have been associated with cardiovascular disease, atherosclerosis, metabolic syndrome, stroke and cerebrovascular disease – and now with autoimmune disease. But why does this occur?  Lipoproteins modulate innate and adaptive immune responses. When cholesterol, LDL (the “bad” cholesterol), and TG are high, there is a “feed-forward mechanism” that essentially sets up a domino reaction and we see increased immune activation, pro-inflammatory cytokines raging, blood-brain barrier (BBB) permeability, microglial activation and more. On the other hand, HDL (the “good” cholesterol) has immunomodulatory and antioxidant effects on endothelial cells and it has been shown to inhibit production of the pro-inflammatory cytokines interleukin-1beta and tumor necrosis factor. So, the working hypothesis is: The pro-inflammatory and thrombogenic processes associated with dyslipidemia (the abnormal level of cholesterol and fats in the blood) could contribute to disease progression in MS and other neurodegenerative diseases via:
In addition, we know that every neurodegenerative harbors mechanisms tied to not just immune dysregulation, but also to mitochondrial health and oxidative stress, which is the imbalance between free radicals and antioxidants in our system. High lipids cause disruption of mitochondrial function and increase oxidative stress. Cumulative oxidative stress may induce cellular damage, impairment of the DNA repair system, and also fuels mitochondrial dysfunction, all of which have been known as key factors in acceleration of the aging process and the development of neurodegenerative disorders. And mitochondrial health has been tied to aging and every neurodegenerative disease as well. Our fatty brain needs fat, but not saturated or trans fats found in the Standard American Diet.  First, a few “fat facts”… The brain is actually a very fatty organ – in fact, it’s made up of an astounding 60% fat! Cholesterol is an important component of intact myelin, the insulating sheath around the nerves. But, while the brain NEEDS fat to function properly, the key is identifying the right kinds of fats. The Standard American diet (SAD) is a recipe for health disaster with its excess of sugar, refined carbohydrates, processed food, fried food, saturated fat and trans fats. We know that the healthiest kind of fats we can eat is unsaturated, found in avocados, nuts, seeds, oily fish, and olive oil. Trans fats, on the other hand, which tend to show up in processed foods like chips, pre-packaged cakes, biscuits, pastries, and ready meals, all negatively affect our health. Saturated fat comes mainly from animal sources of food, such as red meat, poultry and full-fat dairy products. Saturated fats raise high-density lipoprotein (HDL or "good") cholesterol and low-density lipoprotein (LDL or "bad") cholesterol levels. And as just one example of how these negatives fats impact our brain, a Harvard study of 6,000 women published in Annals of Neurology found that those who ate the most saturated fat had the worst memory and thinking ability over time.1 So, what’s the answer and why not put everyone on statins? We know we can't exercise or medicate our way out of a bad diet and unhealthy lifestyles. Dr. Mark Hyman, founder and director of The UltraWellness Center and the Head of Strategy and Innovation at the Cleveland Clinic Center for Functional Medicine says, "It’s not about having lower cholesterol; it’s about having the right type of cholesterol." He also explains “Inflammation is the main cause of heart disease and is what makes cholesterol dangerous.” Likely you are familiar with the use of statin drugs that are so often prescribed to treat high cholesterol. These drugs in a variety of formularies are prescribed to over 200 million people worldwide and are one of the most prescribed medications. However, there is continued controversy as to the benefits of statin therapy for brain health. Statins have been shown to paradoxically increase and decrease brain health - too great a reduction of brain cholesterol with statins that enter the central nervous system might deprive the brain of cholesterol’s beneficial effects. And statins may hinder re-myelination by inhibiting cholesterol synthesis in the brain. Statins, if they do have a good role in brain health it’s probably due to their anti-inflammatory role; some studies have shown an effect on the nervous system in protecting the nerves. Statins also possess immunomodulatory properties, affecting among other processes T cell activation and differentiation, antigen presentation, and regulatory T cell (Tregs) maintenance and differentiation. In MS clinical trials looking at statins as a way to modify brain atrophy and thus disease progression, the effects of a high dose statin therapy was marginal in secondary-progressive multiple sclerosis (SPMS), but showed no benefit in relapsing-remitting multiple sclerosis (RRMS). It’s important to note too that statins are not without side effects that can include muscle pain and damage, liver damage, mitochondrial dysfunction, increased risk of diabetes and other reactions that may impact more seriously certain populations such as elderly people and those with comorbidities.2 Ketogenic Diet in MS.  Ketogenic diets (KD) and fasting diets (FD) as well as fasting-mimicking diets (FMD) drastically reduce carbohydrate intake. It’s been suggested that the resulting ketone bodies that develop with these approaches may facilitate the regeneration of demyelinated axons. Fasting not only induces ketosis, but might also activate autophagy in the brain, liver and muscle. In MS, there is preclinical evidence for the efficacy of KDs and FDs from experimental autoimmune encephalomyelitis (EAE), the established animal model of MS. Studies have found that KD slows disease progression, improves motor disability and hippocampal atrophy, reversed lesions and suppressed inflammatory cytokines and reactive oxygen species. How do KDs and/or FMDs help? 1. Increases mitochondrial density within the body. 2. The body adapts to using ketones rather than glucose for fuels, which eliminates or removes many of the typical sources of chronic inflammation caused by foods. 3. It decreases inflammation by modulating immunity. The FMD reduces pro-inflammatory cytokines and increases corticosterone levels. 4. Some studies suggest FMD/KD may slow the aging process 5. Stimulate signaling pathways within the mitochondria offers neuroprotection 6. FMD promotes regeneration of oligodendrocyte in multiple MS models An interesting study looked at how fasting lowers white blood cell counts, which in turn triggers the production of new white blood cells and strengthens the immune system. The findings, first published June 2014 by Dr. Valter Longo, University of Southern California, who studies aging and longevity, is particularly telling. In this paper, Longo and colleagues described remarkable metabolic changes that occurred as a result of prolonged fasting. They found that fasting for 3 days or longer, drinking only water and eating less than 200 calories per day, can truly “reset” some components of your immune system. Another randomized, controlled clinical study investigated the effects of a KD and a FD compared to a standard diet (SD) in RRMS. Patients in the FD group fasted for 7 days every 6 months. The KD followed a restricted carbohydrate intake of 20–40 g/day; this is the first study that investigates long-term efficacy of keto diet and fasting diet on T2 hyper-intense lesion load and clinical measures of disease activity and progression in MS patients. It’s also the first research that investigated therapeutic effects of repeated prolonged fasting combined with daily intermittent fasting.3 Dr. Longo is conducting even more research on FMDs for brain health. The fasting-mimicking diet aims to reduce the number of proinflammatory T cells, leading to regeneration of myelin. You can read more about Dr Longos work here: https://www.sciencedirect.com/science/article/pii/S2211124716305769 and https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4899145/ A prolonged 4-7 day fast provides health benefits by stressing the body enough to go beyond fat burning associated with reduced calorie intake to cellular regeneration and rejuvenation. To learn more about the L-Nutra’s ProLon 5-day Fasting Mimicking Diet ™ see https://l-nutra.com. Lifestyle modifications that help lower cholesterol. We’ve often written about the impacts of lifestyle choices on many aspects of health and neurological wellness so it’s no surprise that lifestyle modifications can play a significant role in helping to lower cholesterol and potentially reduce the negative impacts to our system. Some of the basic tenets of a beneficial lifestyle approach: 1. Eat heart-healthy, whole foods (preferably organic if available to you and non-GMO). 2. Reduce saturated fats. Saturated fats, found primarily in red meat and full-fat dairy products, raise your total cholesterol (reminder that we typically advise eliminating dairy that may especially exacerbate MS). Decreasing your consumption of saturated fats can reduce LDL levels. While meat contains proteins necessary to build muscle and carry out a variety of functions in the body, unfortunately it also contains varying amounts of cholesterol and saturated fats. Meats that are high in saturated fat content include ground beef, bacon, and organ meats like liver. Meats that are processed, including sausages, hot dogs, and some luncheon meats, are also high in fat and should be consumed in minimal amounts. So concentrate on choosing lean cuts of meats and as well as lower fat poultry. 3. Eliminate trans fats. Trans fats, sometimes listed on food labels as "partially hydrogenated vegetable oil," are often used in margarines and processed foods like store-bought cookies, crackers and cakes. Trans fats raise overall cholesterol levels so much so that the Food and Drug Administration has banned the use of partially hydrogenated vegetable oils by January 2021.4 4. Eat foods rich in omega-3 fatty acids. Omega-3 fatty acids don't affect LDL cholesterol. But they have other heart-healthy benefits, including reducing blood pressure. Foods with omega-3 fatty acids include salmon, mackerel, herring, walnuts and flaxseeds. 5. Increase soluble fiber. Soluble fiber can reduce the absorption of cholesterol into your bloodstream. Soluble fiber is found in such foods as oatmeal, kidney beans, Brussels sprouts, apples and pears. 6. Exercise regularly, choosing any activity to which you can commit and enjoy! Consider outdoor walks and hikes that also give you the benefit of being in nature. Be sure to check with your doctor before beginning any new exercise regimen. 7. Stop smoking – for good. 8. Drink alcohol in moderation 9. Consider a Ketogenic Diet as appropriate to your individual health and under the guidance of your health provider. 10. Lower your stress and find ways to manage situations that cause it. For tips, see our October blog: https://www.suzannegazdamd.com/blog/your-brain-on-stress-and-how-to-conquer-the-effects 11. Lower toxic load. Lead, mercury, and high levels of air pollution have been linked to high lipids. Address chronic infections and pathogens, which drive inflammation which can cause a rise in lipid levels. For more about cholesterol, lipids and MS see our previous detailed blog at: https://www.suzannegazdamd.com/blog/lipids-cholesterol-ms-what-you-need-to-know Here’s to a healthier brain and body that affords you the opportunity to enjoy your life and be part of all the things that bring you great joy! As always, feel free to reach out to our clinics if we can be of any assistance or answer your questions. We are here for you. In health and hope, Dr. Suzanne Gazda References: 1 Chianese, R., Coccurello, R., Viggiano, A., Scafuro, M., Fiore, M., Coppola, G., Operto, F. F., Fasano, S., Laye, S., Pierantoni, R., & Meccariello, R. (2018). Impact of Dietary Fats on Brain Functions. Current neuropharmacology, 16(7), 1059–1085. https://doi.org/10.2174/1570159X15666171017102547 2 Mayo Clinic: statin side effects. https://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/in-depth/statin-side-effects/art-20046013 3 Bahr, L. S., Bock, M., Liebscher, D., Bellmann-Strobl, J., Franz, L., Prüß, A., Schumann, D., Piper, S. K., Kessler, C. S., Steckhan, N., Michalsen, A., Paul, F., & Mähler, A. (2020). Ketogenic diet and fasting diet as Nutritional Approaches in Multiple Sclerosis (NAMS): protocol of a randomized controlled study. Trials , 21(1), 3. https://doi.org/10.1186/s13063-019-3928-9 4 Food and Drug Administration determination. https://www.fda.gov/food/food-additives-petitions/final-determination-regarding-partially-hydrogenated-oils-removing-trans-fat
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorDr. Suzanne Gazda, Integrative Neurology Archives
February 2024
Categories |
 RSS Feed
RSS Feed