|
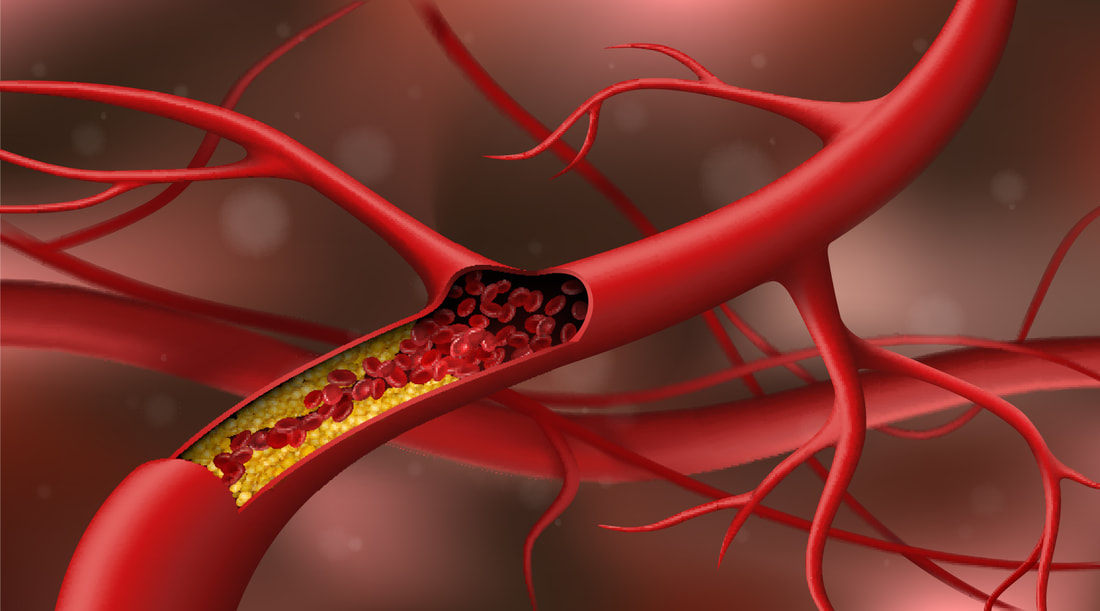
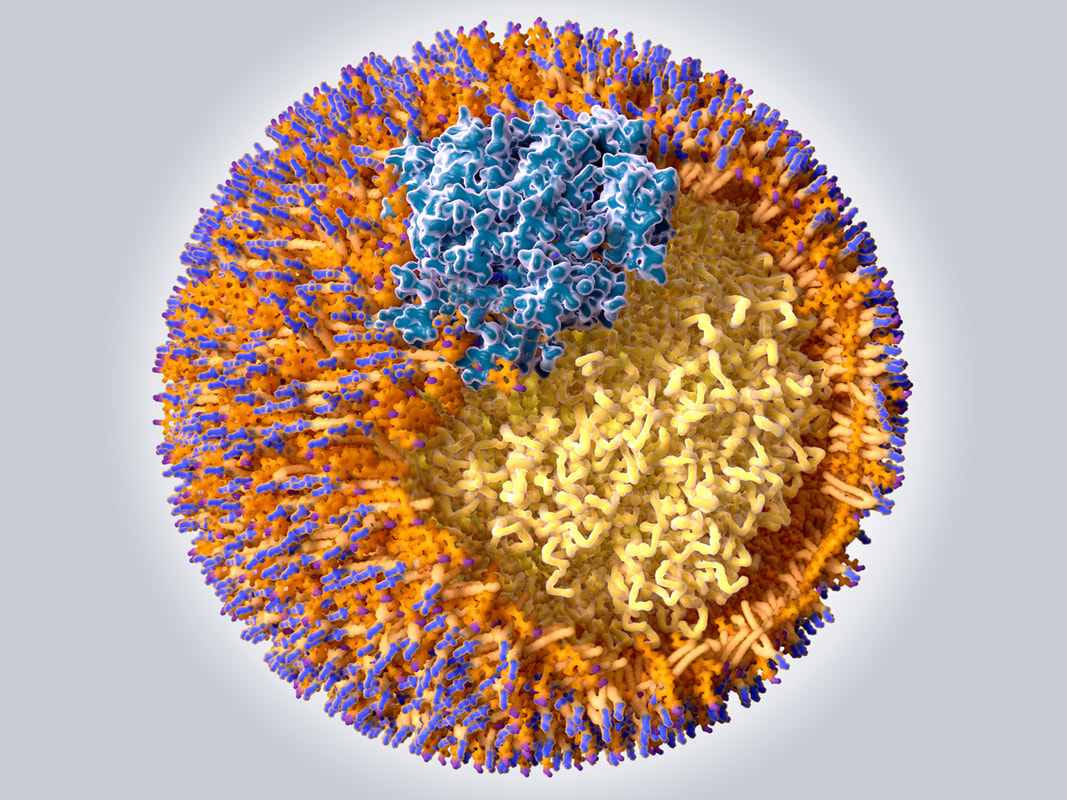
We know that it’s important to be aware of our cholesterol levels – but now studies are providing even more information about the mechanisms that link cardiovascular disease (CVD) AND neurodegenerative disorders. Dyslipidemia, which refers to abnormally elevated cholesterol or fats (lipids) in the blood, is a well-recognized player in atherosclerosis and in the vascular inflammation underlying CVD. In recent years it has been suggested to also play a role in multiple sclerosis (MS) as new research highlights the correlation of cholesterol to MS and especially in MS fatigue. What is Cholesterol? Just like other basic food components, cholesterol is an essential component in a healthy human body. It forms the cell membrane architecture (or the cell wall), helps produce the sex hormones, and assists in the formation of bile that is inherent to the digestion of food. It is important to understand that your own body naturally produces cholesterol in the liver, in addition to what is consumed in your diet. Plants, on the other hand, cannot produce cholesterol – and that’s why it’s important to note that the largest dietary sources of cholesterol are meat and dairy products. Cholesterol travels through the bloodstream attached to low-density lipoprotein (LDL) “bad cholesterol” and high-density lipoprotein (HDL) “good cholesterol.” In conjunction with these types of cholesterols are triglycerides, which are the most common type of fat in the body. A high triglyceride level combined with high LDL or low HDL (good) cholesterol is linked with fatty buildups within the artery walls, which increases the risk of heart attack and stroke. It’s also important to understand the role of triglycerides, the most common type of fat in the body. According to the American Heart Association, a high triglyceride level combined with high LDL or low HDL (good) cholesterol is linked with fatty buildups within the artery walls, which then increases the risk of heart attack and stroke. Optimum cholesterol levels Total cholesterol should be under 200. Triglycerides should be under 100. HDL should be over 60. LDL should be ideally under 80. Ratio of total cholesterol to HDL should be less than 3.0. Ratio of triglycerides to HDL should be no greater than 4, which can indicate insulin resistance if elevated. Do lipid panels give us all the information we need? Hypercholesterolemia, hypertriglyceridemia, elevated low-density lipoprotein cholesterol (LDL-C), and low high-density lipoprotein cholesterol (HDL-C) are generally accepted as strong risk factors for CVD and mortality. However, just looking at basic lipid markers such as your overall cholesterol and triglycerides, is sometimes not that helpful given that roughly 50% of people that have heart attacks actually have normal cholesterol levels. Dr. Mark Hyman, founder and director of The UltraWellness Center and the Head of Strategy and Innovation at the Cleveland Clinic Center for Functional Medicine says "It’s not about having lower cholesterol; it’s about having the right type of cholesterol." He also explains “Inflammation is the main cause of heart disease and is what makes cholesterol dangerous. Inflammation can arise from poor diet (too much sugar and trans and saturated fats), a sedentary lifestyle, stress, autoimmune disease, food allergies, or hidden infections such as gum disease, or even toxins such as mercury."1 However, results from a number of studies have indicated that the biomarker apolipoprotein B (ApoB), apolipoprotein A1 (ApoA1), and ApoB/ApoA1 ratio could improve the prediction of CVD and mortality in comparison with total cholesterol, HDL-C, and LDL-C. ApoB has come to the forefront as being a better representation of the number of cholesterol-laden particles circulating in the bloodstream. An inexpensive assay for this blood protein therefore may be the most important test to consider given that it can clearly show the number of these cholesterol-laden particles circulating in the blood, which some researchers believe is a truer indicator of the threat to our arteries than absolute cholesterol levels. Lipids in MS. In MS higher total cholesterol and LDL-cholesterol levels have been linked to worsening disability, with greater ApoB levels at disease onset being linked to increased number of lesions on MRI brain scans over a two-year period.2 Increases in HDL‐C (which ideally should be greater than 60) and ApoA‐I (should be greater than or equal to 14) have protective associations with magnetic resonance imaging (MRI) measures of neurodegeneration in MS. But, elevated levels of circulating low density lipoprotein cholesterol (LDL), total cholesterol, and particularly, apolipoprotein B and oxidized LDL are associated with adverse clinical and MRI outcomes. In an extensive study, researchers reviewed the longitudinal changes of cholesterol biomarkers (total cholesterol, HDL-C, LDL-C, Apo profiles and their genotyping) over a 5 year period in healthy subjects and MS, and their relationship with brain lesions and volume loss. The study involved 41 healthy controls (HC), 76 relapsing-remitting MS (RR-MS), and 37 progressive MS (P-MS) subjects. They found that, while a rise in LDL-C was associated with the development of new MS lesions, HDL-C and ApoA-I (a component of HDL-C) were associated with less grey matter and cortical volume loss (the area of the brain where the neuronal cell bodies sit). The highest quartiles of LDL-C were linked to the greatest number of new MS lesions. The opposite was true for HDL-C, with the lowest quartile of HDL-C change being associated with more gray matter and cortical volume loss. Both findings imply that extremes in change to high or low levels are somehow very harmful. MS and fatigue: reduced fatigue, improved lipid panels. Total cholesterol or TC to HDL-C ratio is an important number to know; the higher the ratio, the higher the risk. Most healthcare providers want the ratio to be below 5:1. A ratio below 3.5:1 is considered to be very good. To calculate your cholesterol ratio, divide your total cholesterol number by your HDL cholesterol number. So if your total cholesterol is 200 mg/dL (5.2 mmol/L) and your HDL is 50 mg/dL (1.3 mmol/L), your ratio would be 4-to-1. Remember that higher ratios mean a higher risk of heart disease! We know too that TC to HDL-C ratio is associated with MS fatigue. Recent findings implicate a potential role for the HDL-C pathway in MS fatigue and could provide possible targets for the treatment of MS fatigue.3 This may be another mechanism in which plant-rich diets like the Wahls protocol improve fatigue symptoms in MS.4 Higher levels of HDL had the greatest impact on fatigue and this is possibly because good cholesterol plays a critical role in muscle, stimulating glucose uptake and increasing respiration in cells to improve physical performance and muscle strength. Healthy body, healthy brains! When we look at all the research and the findings, a common thread stands out – that in order to have a healthy brain and prevent or reduce symptoms in many neurodegenerative diseases like MS, we MUST first strive for a healthy lifestyle that supports our entire system. That means shoring up our immune defenses as well as our gut and metabolic functions sound lifestyle choices and optimal nutrition, avoiding highly inflammatory foods, managing stress and, of course, getting that much-needed rest. Your healthcare practitioner is an excellent resource for information as to how you can achieve results consistent with your individual health needs. And of course we are always happy to provide additional guidance - so don’t hesitate to reach out to our clinics for more details about our comprehensive and individualized integrative protocols. We are here to help! In health and hope, Dr. Suzanne Gazda References and additional reading: 1 The Cholesterol Solution, Mark Hyman MD https://drhyman.com/blog/2016/01/14/7-ways-to-optimize-cholesterol/ https://drhyman.com/wp-content/uploads/2018/02/The-Cholesterol-Solution_ebook_022318.pdf?v=1.1 2 Browne RW, Weinstock-Guttman B, Horakova D, Zivadinov R, Bodziak ML, Tamaño-Blanco M, Badgett D, Tyblova M, Vaneckova M, Seidl Z, Krasensky J, Bergsland N, Ramasamy DP, Hagemeier J, Havrdova E, Ramanathan M. Apolipoproteins are associated with new MRI lesions and deep grey matter atrophy in clinically isolated syndromes. J Neurol Neurosurg Psychiatry. 2014 Aug;85(8):859-64. doi: 10.1136/jnnp-2013-307106. Epub 2014 Jan 27. PMID: 24470599. 3 Browne, R. W., Jakimovski, D., Ziliotto, N., Kuhle, J., Bernardi, F., Weinstock-Guttman, B., Zivadinov, R., & Ramanathan, M. (2019). High-density lipoprotein cholesterol is associated with multiple sclerosis fatigue: A fatigue-metabolism nexus? Journal of clinical lipidology, 13(4), 654–663.e1. https://doi.org/10.1016/j.jacl.2019.06.003 https://pubmed.ncbi.nlm.nih.gov/31307953/ 4 University at Buffalo. (2019, August 15). Vegetable-rich diet lowers fatigue in multiple sclerosis patients by raising good cholesterol: Fatigue affects majority of MS patients, impacting quality of life and ability to work full time. ScienceDaily. Retrieved October 22, 2020 from www.sciencedaily.com/releases/2019/08/190815134822.htm
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorDr. Suzanne Gazda, Integrative Neurology Archives
February 2024
Categories |
||||||
 RSS Feed
RSS Feed