|
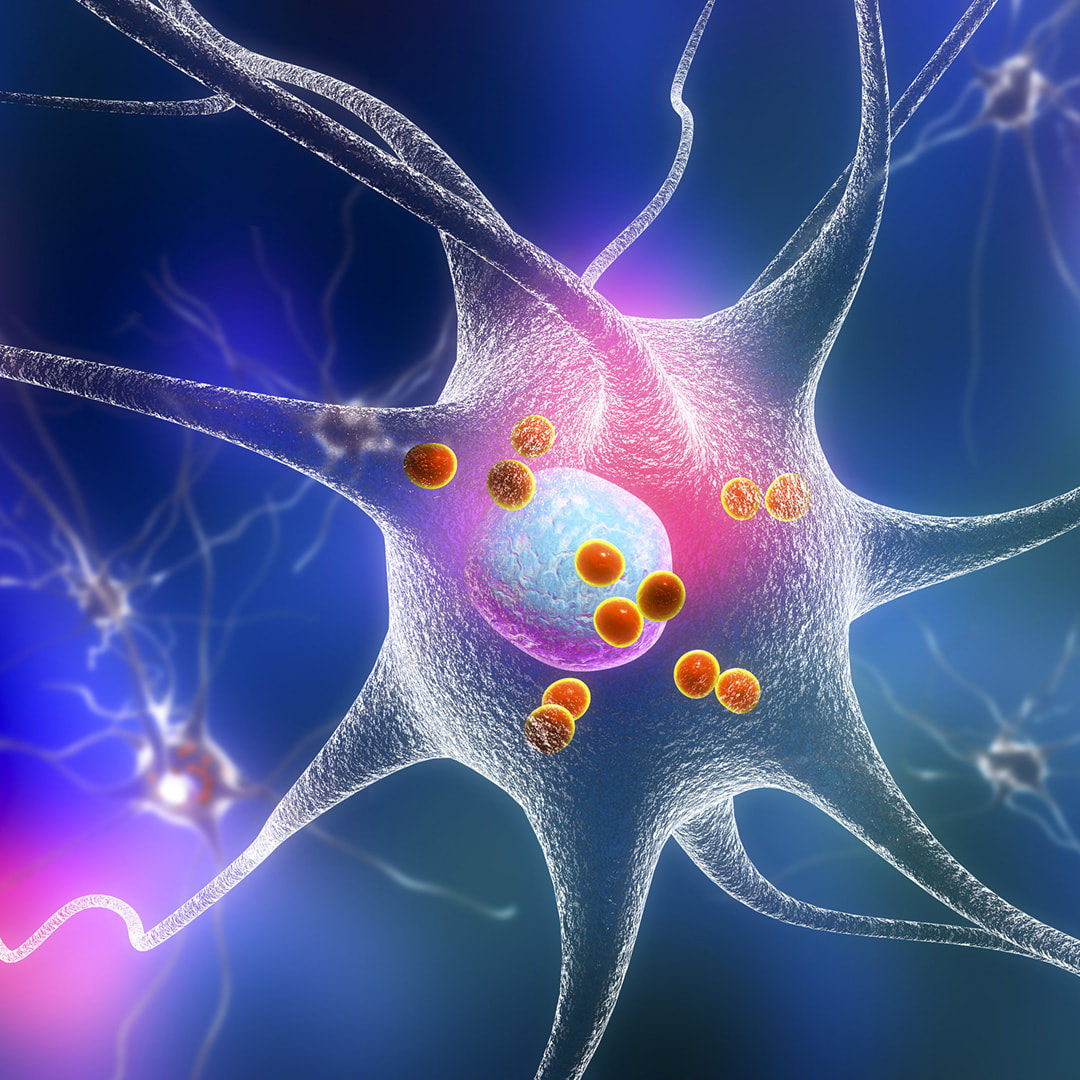
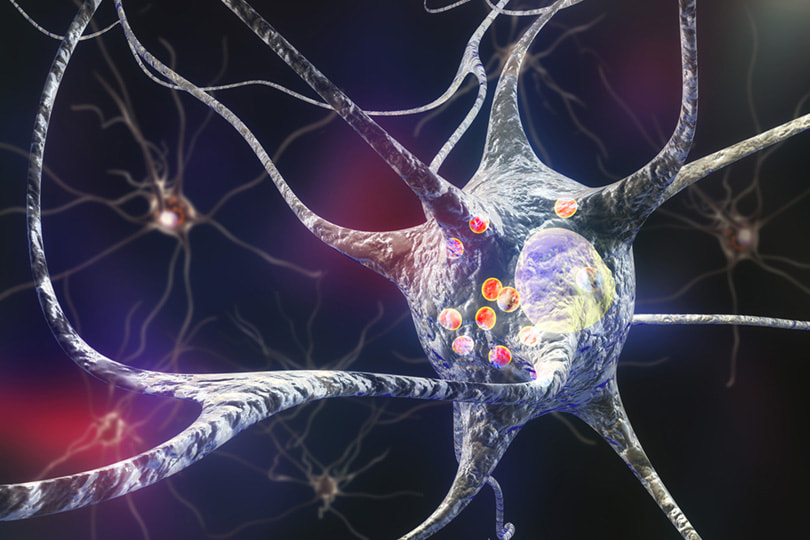
For many years, researchers have studied the role of autoimmunity in Parkinson’s disease (PD) and there is ample evidence that what we know to be drivers of autoimmune disease may very well play a role in this neuromuscular condition. As we have often discussed, there are certain predicating factors including environmental concerns and exposures to toxic elements that can contribute to the dysfunction of our immune system. So, could a neurological disorder like PD be influenced by these same factors? Let’s look at the research… Scientists have focused on autoimmunity and found it is actively involved in the pathogenesis of PD through several proteins, including alpha-synuclein (α-Syn), DJ-1, PINK1, and Parkin, as well as immune cells, such as dendritic cells, microglia, T cells, and B cells.1 We know that clumps of the damaged α-Syn protein can build up in the dopamine-producing brain cells of patients with Parkinson's disease. As a neurotransmitter, dopamine is especially susceptible to the effects of these clumps that may eventually lead to cell death, presentation of impaired motor processes and cognitive decline. A small synaptic protein and the primary component of Lewy bodies, α-Syn can, if incorrectly modified or misfolded, form soluble or insoluble aggregates and act as the neuropathological hallmark in the brain of patients with either sporadic or familial PD. Equally significant is to note is that the formation and aggregation of misfolded proteins in the central nervous system (CNS) is a key hallmark of not only Parkinson’s disease (PD), but also Alzheimer’s disease (AD), and amyotrophic lateral sclerosis (ALS).2 α-Syn plays a leading role in the initiation and progression of Parkinson-like neurodegeneration because it can induce high neurotoxicity by diverse pathways, such as inflammation, oxidative stress and autophagy abnormalities. Particularly important, studies have provided extensive evidence that indicates “abnormal α-Syn can spread to neighboring brain regions and cause aggregation of endogenous α-syn in these regions as seeds, in a “prion-like” manner.”3
These findings may well point to an underlying autoimmune response that develops before the formation of these prions, further fueling the fire of chronic neuroinflammation.4 As for more evidence? In another recent publication, we learn that it is dysregulation of the immune system in conjunction with genetic mutations and environmental factors are contributing pathogenic factors in the initiation of PD. And we know that high levels of chronic neuroinflammation lead to neurodegeneration. This study demonstrates that subsets and cytokine expression profiles of peripheral adaptive immune cells in patients with early-stage PD show distinct differences compared with HCs matched for age and sex. These peripheral abnormalities may drive PD disease initiation and progression through enhanced infiltration of immune cells and enhanced neuroinflammation in the CNS.5 There are many, many factors involved in what we believe may drive autoimmune disease and that should be spotlighted in order to best address overall toxic load and environmental health. As we’ve previously written, it may be that other diseases, such as Alzheimer’s, also prove to have autoimmune origins. So it’s truly in our best interests that we continue to study the autoimmunity aspects of neurological disease in order to identify our risks and develop more efficacious treatments. With new findings comes more hope that doctors will one day have the means to make earlier diagnoses of Parkinson’s disease that subsequently leads to earlier intervention. In health and hope, Dr. Suzanne Gazda References: 1 Jiang T, Li G, Xu J, Gao S, Chen X. The Challenge of the Pathogenesis of Parkinson's Disease: Is Autoimmunity the Culprit? [published correction appears in Front Immunol. 2019 Oct 16;10:2242]. Front Immunol. 2018;9:2047. Published 2018 Sep 27. doi:10.3389/fimmu.2018.02047 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6170625/ 2 Cecilia S. Lindestam Arlehamn, Rekha Dhanwani, John Pham, Rebecca Kuan, April Frazier, Juliana Rezende Dutra, Elizabeth Phillips, Simon Mallal, Mario Roederer, Karen S. Marder, Amy W. Amara, David G. Standaert, Jennifer G. Goldman, Irene Litvan, Bjoern Peters, David Sulzer, Alessandro Sette. α-Synuclein-specific T cell reactivity is associated with preclinical and early Parkinson’s disease. Nature Communications, 2020; 11 (1) DOI: 10.1038/s41467-020-15626-w 3 Kumar, S., Thangakani, A., Nagarajan, R. et al. Autoimmune Responses to Soluble Aggregates of Amyloidogenic Proteins Involved in Neurodegenerative Diseases: Overlapping Aggregation Prone and Autoimmunogenic regions. Sci Rep 6, 22258 (2016). https://doi.org/10.1038/srep22258 4 Ma J, Gao J, Wang J and Xie A (2019) Prion-Like Mechanisms in Parkinson’s Disease. Front. Neurosci. 13:552. doi: 10.3389/fnins.2019.00552 5 Zhaoqi Yan, Wei Yang, Hairong Wei, Marissa N. Dean, David G. Standaert, Gary R. Cutter, Etty N. Benveniste, Hongwei Qin. Dysregulation of the Adaptive Immune System in Patients With Early-Stage Parkinson Disease. Neurol Neuroimmunol Neuroinflamm Jul 2021 8 (5) e1036; DOI: 10.1212/NXI.0000000000001036
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
Authorby Suzanne Gazda M.D. Archives
August 2021
Categories |
 RSS Feed
RSS Feed