|
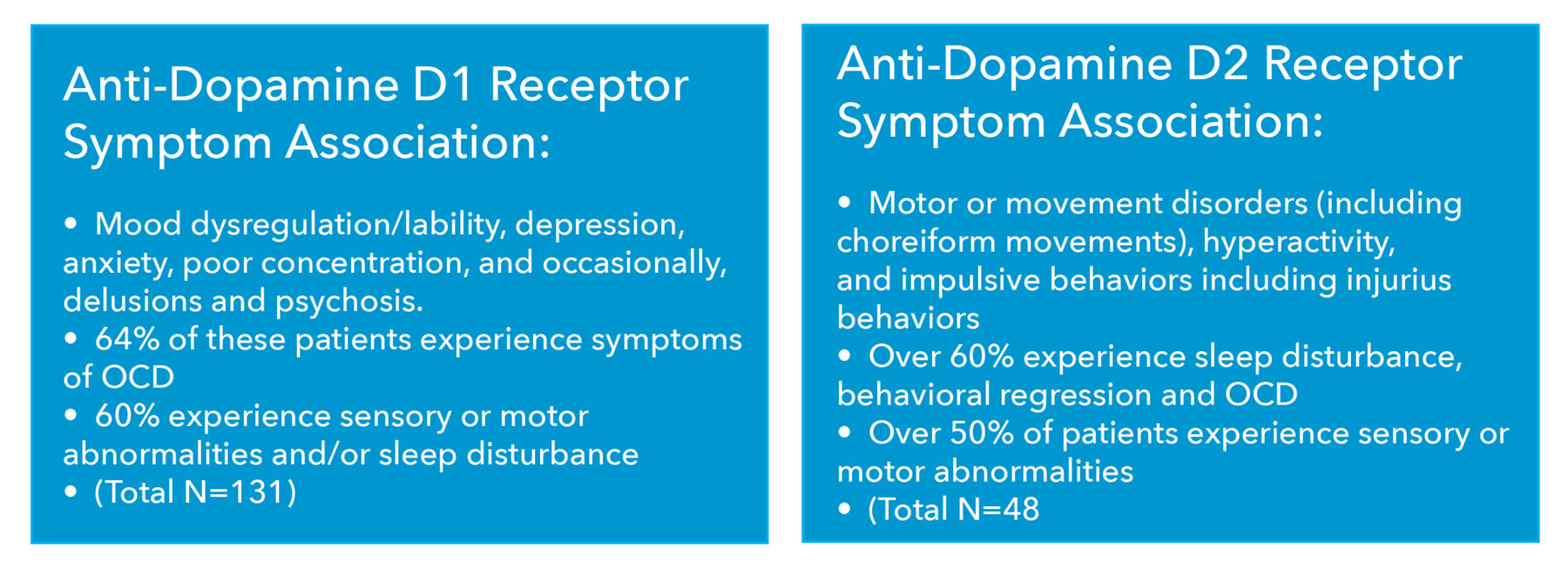
We recently read a brilliant article that sheds more light on the dysregulated immune system that occurs in numerous autoimmune-driven neurological illnesses including: ~ Pediatric acute-onset neuropsychiatric syndrome (PANS) ~ Pediatric autoimmune neuropsychiatric disorders associated with streptococcus (PANDAS) ~ Basal ganglia encephalitis (BGE) ~ Autoimmune encephalitis (AE) ~ Movement disorders ~ Other autoimmune driven neurological diseases like multiple sclerosis (MS, neuromyelitis optica spectrum disorder (NMOSD) and a subset of neuropsychiatric conditions from obsessive compulsive disorder to ADHD, depression, anxiety and more. The research and immune responses. In this exceptionally well designed study published in Clinical and Translational Immunology, scientists explored the dysregulated inflammatory response against dopamine-2 receptors (D2R), which are implicated in these movement and neuropsychiatric disorders. Basically, dopamine receptors are involved in many neurological processes; subsequently, ABNORMAL dopamine receptor signaling and dopaminergic nerve function that is triggered by infectious agents are often associated with a number of neuropsychiatric disorders in children and adults. It’s a complicated interaction that starts with the D2R, which is abundantly expressed in the basal ganglia, limbic system and cerebral cortex that are responsible for movement, motivation, learning, emotions and memory. D2Rs are also present on immune cells and work to help modulate the immune system in the peripheral nervous system. Dopaminergic signaling can modulate immunological processes, such as T- and B-cell interactions in antibody production, activation of naïve T-cells, inhibition of stimulated T-cells, suppression of regulatory T-cells, cytokine secretion, as well as cellular trafficking and chemotactic migration or chemotaxis of T cells. Chemotaxis refers to the migration of cells toward attractant chemicals or away from repellents; virtually, every motile organism exhibits some type of chemotaxis.1 Cytokines are the “chemical messengers” responsible for most of the biological effects in the immune system and T lymphocytes are a major source of cytokines. So, in patients with a dysregulated immune response directed to the DR2R, “the perfect storm” develops that cascades down the road of not only neurological or neuropsychiatric symptoms, but also propagation of neuropathology leading to irreversible and progressive symptomatology. We have in the past discussed DR2-directed autoantibodies and how this blocking mechanism on the receptor can cause a cascade of symptoms as well, but in this study the focus was not on antibodies (there were none), but rather on the autoreactive T-cell response against D2R. These T-cells are associated with a Th1 and Th17 phenotype, suggesting a T-cell-driven immune response. Th1 cells stimulate cellular immune response, participate in the inhibition of macrophage activation and stimulate B cells to produce IgM, IgG1. Th2 cells stimulate humoral immune response, promote B cell proliferation and induce antibody production. What this study clearly showed was that even in the absence of DR2 receptor antibodies, it is the pathologic immune dysregulation that is driving symptoms and brain pathology. These activated D2R-specific T cells are being fueled by reactions with their antigenic counterpart along with an inflammatory cascade of cytokines and activation of complement systems which are play a major role in the innate immune system. The innate immune responses are the first line of defense against invading pathogens. Molecular mimicry fueling the fire (again!).
Many believe that these mechanisms are infectious-driven through the process of molecular mimicry whereby cross-reactivity between microbial structures and host proteins results in an immune response misdirected to the host. This could very well be the reason why in PANS and PANDAS (and even in some cases of MS) we may see disease exacerbation when there is an underlying infectious trigger. And this also could explain the negative Cunningham panels we see in some of our PANS and PANDAS patients as it also clarifies more about the other mechanisms driving these “brains on fire.” Summing up the significance of these findings… The results present several key items: ~ Study authors noted the presence of peripheral autoreactive T cells against D2R that were not associated with autoantibodies in patients with neurologic and psychiatric symptoms. ~ This sheds more light on disease mechanisms and neural signaling issues that better explains the mechanisms of disease. ~ Findings continue to support the enormity of early identification and diagnosis as well as appropriate treatment and intervention – truly, we cannot emphasize this enough! ~ Early treatment utilizing IVIg in some cases of PANS and PANDAS may aid in the “immune response reset” that could dampen or even stop the progression of “brain on fire.” Bottom line... it is not always streptococcus bacteria at work and ALL potential infectious and non-infectious triggers must be explored. The stark reality is that in many instances by the time patients come to us, the infectious trigger is long gone and it is the immune dysregulation that must be stabilized and improved. And we already know that epitope (the part of an antigen molecule to which an antibody attaches itself) spreading is known to advance disease in MS and in most autoimmune diseases.2 I believe what is missing in most protocols is a well designed and individualized neuroplasticity protocol. And sadly, we are simply getting many of these cases in an advanced state of disease. So we are especially grateful for research that will lead to more patients receiving accurate timely diagnoses and comprehensive, integrative care that is appropriate to their specific health needs. Let’s hope that the science continues to progress toward providing the best practices resolutions for the wellbeing of all those who struggle with these highly complex and destructive disorders. So many patients and their families are counting on all of us! In health, Dr. Suzanne Gazda References: 1 J.B. Stock, M.D. Baker. Encyclopedia of Microbiology (Third Edition). 2009 2 Shivaprasad H. Venkatesha, Malarvizhi Durai, Kamal D. Moudgil. Chapter 4 - Epitope Spreading in Autoimmune Diseases. Editor(s): Yehuda Shoenfeld, Nancy Agmon-Levin, Noel R. Rose. Infection and Autoimmunity (Second Edition) 2015, Academic Press. Pages 45-68. ISBN 9780444632692. https://doi.org/10.1016/B978-0-444-63269-2.00003-9. For additional articles about PANS and PANDAS, please see these selections below or use the “search” bar function on our website to explore the library of materials and information. https://www.suzannegazdamd.com/blog/pans-and-pandas-is-making-the-newsbut-what-do-we-really-know https://www.suzannegazdamd.com/blog/why-is-nutrition-so-important-in-pans-and-pandas
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
Authorby Suzanne Gazda M.D. Archives
August 2021
Categories |
 RSS Feed
RSS Feed