And when gadolinium is used as a contrast agent in some of these tests, it’s especially important to be aware of the potential negative and neurotoxic impacts that can emerge post-administration.
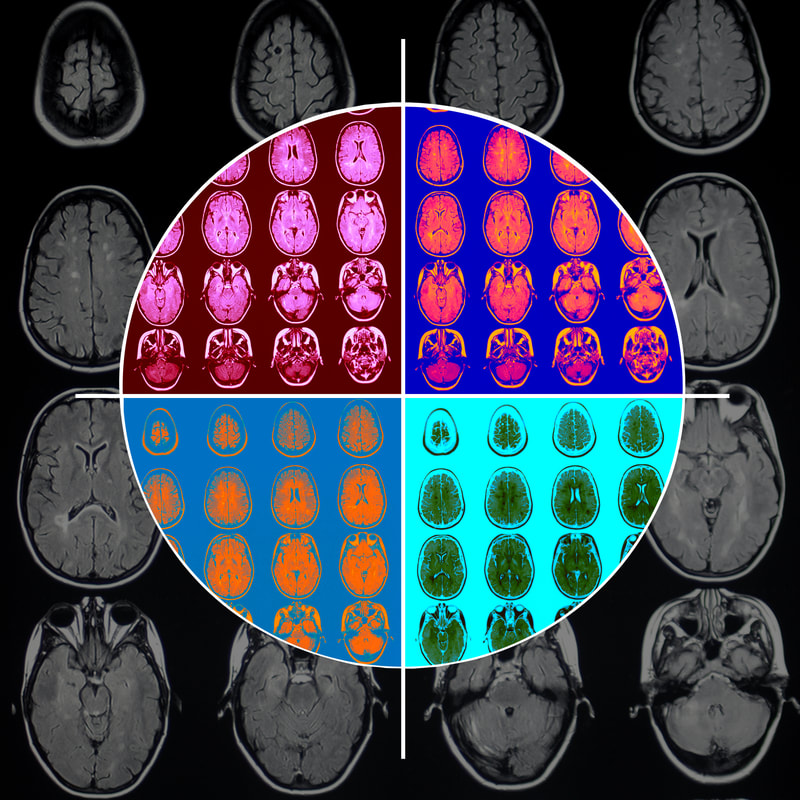
In 2017, the Food and Drug Administration demanded that more reviews be conducted on the safety of this agent that was first introduced for use almost 30 years ago based on the variety of issues that can arise in some patients.1 We know that gadolinium inhibits mitochondrial function and induces oxidate stress; when mitochondrial dysfunction occurs it can create neural inflammation and conversely the inflammation can also cause mitochondrial dysfunction. This is especially of concern when looking at neurological disease and noting that patients may after a contrast MRI experience symptoms such as headache, confusion, dizziness, and bone and limb pain – while these may be relatively nonspecific or even go unnoticed, there are numerous cases of gadolinium toxicity that have been reported. Patients with reduced kidney function, acidosis, inflammatory events, vascular disease, or compromised blood-brain barrier do appear to be more at risk for complications from a contrast MRI. Additional issues of note: - Repeat contrast MRIs and subsequent cumulative doses of the gadolinium agent can cause other problems. Physicians may order these types of imaging studies over a six-month period, for example, when monitoring for disease progression as the gadolinium will enhance “active” MS lesions due to a breakdown in the blood-brain barrier. A recent study found a correlation between higher T1 signal intensity in the dentate nucleus and lower verbal fluency after correcting for disease severity. - Transmetalation is perhaps the biggest risk factor after kidney impairment; many patients we see today exhibit high levels of toxic metals that accumulate from many sources including our water supply, vaccines, air pollution, food and other environmental influences. Let’s look at some of the science. The study, “Gadolinium-Based MRI Contrast Agents Induce Mitochondrial Toxicity and Cell Death in Human Neurons, and Toxicity Increases with Reduced Kinetic Stability of the Agent.” For the study, neurons modeling a subset of those in the basal ganglia were tested given that the basal ganglia region is one of two brain regions that displays the greatest T1-dependent signal hyper-intensity changes. Many studies have shown that T1-signal intensity changes in the brain are the result of gadolinium deposition. The authors noted that there is increasing evidence that all agents (linear and macrocyclic) remain in human brain tissue for some period of time, where they may be taken up into various cell types, including glia and neurons.2 In another recent investigation, “Cumulative gadodiamide administration leads to brain gadolinium deposition in early MS” (https://n.neurology.org/content/93/6/e611) gadolinium was seen in the brains of MS patients early in their disease course as opposed to the brains of the control group. These newly diagnosed MS patients were followed over a 4.5 year period and received an average of 9.2 gadolinium injections. The investigators here found that the gadolinium deposition did NOT affect MS severity. However, I don’t believe that following these study participants for only 4.5 years was necessarily long enough to arrive at this determination. The researchers did identify that MS patients who had received more than 9.2 injections of gadodiamide tended to have a higher number of brain lesions, as well as more severe brain atrophy compared to those who had less than 9.2 gadodiamide administrations. At the same time, 8.9% of MS patients who received fewer than five doses did have hyperintensity in the part of the brain, called the dentate nucleus, involved in voluntary motor function and cognition, which is often affected by MS; none of the healthy controls exhibited this same response. Often, when we look at studies that may appear to offer conflicting interpretations or even very different information, one thing that that stands out is just how important it is that more extensive investigations are done. But I do think that in general it’s best to exercise caution if ordering MRIs plus gadolinium, especially in patients with known neurological or serious underlying health conditions. So what is an alternative to traditional contrast MRIs? In my practice, I almost exclusively use NeuroQuant® (NQ) with CorTech Labs software. A type of MRI, it is FDA-approved and has been widely employed by hospitals, radiologists and imaging facilities in the U.S. and other countries. NQ uses quantitative analysis to visualize roughly 60 different brain regions and measures structural volumes and then uses normative reference data to compares your results to someone your age and gender. NQ is highly reliable with the earlier approach based on computer-assisted, manual identification of brain regions, but without the use of gadolinium. In MRIs, radiologists’ interpretations were based on simple visual inspection, not qualitative ratings that can provide us with a wider spectrum of information and detail. NQ may also be a better way to assess gray matter atrophy, as we discussed in more detail in this article. Current clinical applications of NQ range from evaluation of mild cognitive impairment (MCI) to dementia, epilepsy, and multiple sclerosis, as well as traumatic brain injury (TBI), depression, post-traumatic stress disorder and other neurodegenerative diseases such as Huntington’s chorea and Parkinson’s disease. Biomarkers such as the volumetric measurement of the hippocampus by magnetic resonance imaging (MRI) and NQ are increasingly becoming an important potentially predictive tool for early diagnosis in Alzheimer’s disease (AD). I believe the NQ also has predictive capabilities and can provide us with even more detailed information relevant to all brain diseases. There are some key components in designing integrative neurology care plans for all of our patients that address neuroplasticity treatment strategies, approaches such as The Bredesen Protocol, Wahls Protocol and a vigorous search for the root cause of any neurodegenerative disease. And in treatment paradigms for multiple sclerosis, these are all very much needed. The benefits of an integrative approach enable us to be very individualized in our recommendations, from assessments to comprehensive care that considers every lifestyle and other factors. It’s important to note that what may not be advisable for some patients based on their medical history or comorbidities may be very appropriate in another patient’s plan. As always, don’t hesitate to let us know if you have any questions or if we can help in any way. Zivjio, ( “to a long life”, as my wonderful Czech grandparents would say!) Dr. Suzanne Gazda References: 1 FDA Drug Safety Communication: FDA warns that gadolinium-based contrast agents (GBCAs) are retained in the body; requires new class warnings. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-gadolinium-based-contrast-agents-gbcas-are-retained-body 2 Bower DV, Richter JK, von Tengg-Kobligk H, Heverhagen JT, Runge VM. Gadolinium-Based MRI Contrast Agents Induce Mitochondrial Toxicity and Cell Death in Human Neurons, and Toxicity Increases With Reduced Kinetic Stability of the Agent. Invest Radiol. 2019;54(8):453-463. doi:10.1097/RLI.0000000000000567 https://pubmed.ncbi.nlm.nih.gov/31265439/ For more information about NeuroQuant: https://www.cortechslabs.com/products/neuroquant/
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorDr. Suzanne Gazda, Integrative Neurology Archives
February 2024
Categories |
 RSS Feed
RSS Feed