|
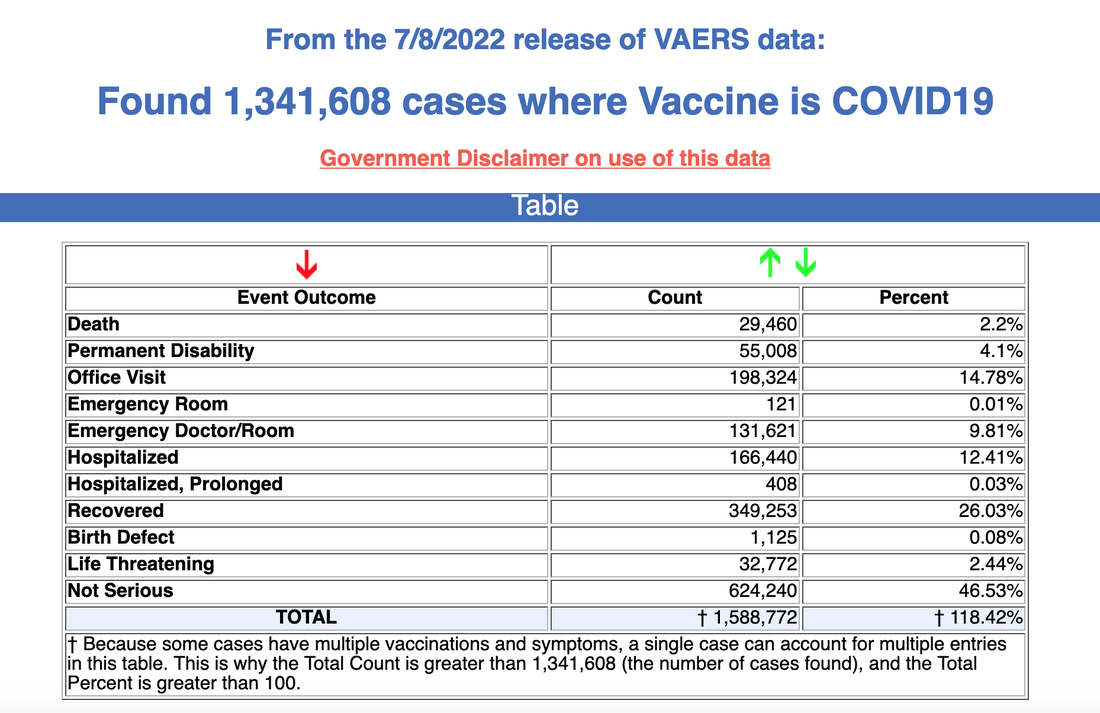
Extended COVID-19 symptomatology over weeks to months is now recognized as long COVID or post-acute COVID-19 syndrome or PASC (post-acute sequelae of COVID). Those individuals who were previously ill with even mild infections can develop lingering, sometimes debilitating, symptoms and become unable to work or even care for themselves. There are instances of long COVID occurring in vaccinated patients who become infected with the virus and in some cases, issues similar to those of long COVID also may develop as a side effect of the COVID vaccine. The Vaccine Adverse Event Reporting System (VAERS), administered by the Centers for Disease Control and Prevention (CDC) shows a total of 1,301,356 reports of adverse post-vaccine events submitted between December 14, 2020 and June 10, 2022. How many are suffering? In the U.S. alone, roughly one in five adults with a known previous case of COVID-19 currently has long COVID symptoms, according to recent data from the National Center for Health Statistics. But other studies are showing even more dismal numbers. Some researchers estimate that fewer than 10% of COVID infections progress to long COVID[FG1] , while others approximate the rate at more than half. In children and adolescents, the reported prevalence varies even more widely—between 4% and 66%, according to a review of 14 studies. In the largest study of its kind, published recently in BMJ, researchers estimated that “32% of older adults in the U.S. who survived COVID infections had symptoms of long COVID up to four months after infection — more than double the 14% rate an earlier study found in adults ages 18 to 64.” There also are other studies that suggest symptoms can last much longer, for a year or more. A recent investigation conducted in the United Kingdom showed seven out of ten patients experiencing long COVID symptoms were experiencing cognitive problems. Bottom Line: This is the Pandemic upon the Pandemic… and untold numbers are suffering . No End in Sight. We continue to see rising cases of COVID 19; therefore, given the scale of the pandemic with at least 90 millionreported cases, even a low percentage of a post COVID outcome of long COVID will generate a frightening tsunami of health problems. Initial indications suggest that the likelihood of developing persistent symptoms may not be related to the severity of the initial illness; it is even conceivable that infections that were initially asymptomatic could later cause persistent problems. Given that many infections are not reported, blood antibody tests suggest that 187 million Americans had gotten the virus by February 2022, according to the CDC. Recently noted in a news release, “as COVID-19 cases continue to rise in the Americas, with new infections increasing by 13.9% from last week, Pan American Health Organization (PAHO) Director, Carissa F. Etienne has called for countries to prepare their health systems to address the long-term impact of post-COVID condition (commonly known as long COVID), which may impact many in the region.” More infections will mean more and more cases of long COVID. A preprint of a study published earlier this month on Research Square found that risk of long COVID, hospitalization, and death increased with each COVID reinfection. This large study done at the Veterans Administration showed these findings: a. The cumulative risks of repeated infection showed that the risk and burden increased in a graded fashion according to the number of infections. b. One or two or more vaccines did not change the outcome. c. Reinfection contributes additional risks of all-cause mortality, hospitalization, and adverse health outcomes in the pulmonary and several extrapulmonary organ systems. Unlike the common cold or even influenza, this virus causes a bewildering array of symptoms that persist long after the acute illness is resolved and can render some affected unable to resume their usual activities. According to the CDC, there are a myriad of possible post-COVID issues that have been reported following an infection; at this time there are a number of most-common symptoms, and other conditions that have followed an infection, but may not necessarily be a direct result of having been infected. The complexity of the syndrome and its many impacts will have to be further investigated to best understand the full implications. Some commonly reported problems: Tiredness or fatigue that interferes with daily life Symptoms that get worse after physical or mental effort (also known as “post-exertional malaise”) Fever Difficulty breathing or shortness of breath Cough Shortness of breath Chest pain Fast-beating or pounding heart (also known as heart palpitations) Difficulty thinking or concentrating (sometimes referred to as “brain fog”) Headache Sleep problems Dizziness when you stand up (lightheadedness) Pins-and-needles feelings Brain fog and cognitive impairment Tremor/abnormal movements Extreme fatigue Change in smell or taste Depression or anxiety Diarrhea Stomach pain Joint or muscle pain Rash Changes in menstrual cycles Vertigo/dizziness Loss of smell and/or taste Other less frequently reported issues: New onset diabetes, heart problems, endocrine disease Autoimmune disease Stroke, clotting, bleeding Cancer and other conditions. Disability policy experts have long-warned that the COVID-19 pandemic would likely be a mass disabling event. New analysis of the U.S. Bureau of Labor Statistics’ (BLS) data on the civilian, non-institutional population aged 16 years and over shows that, in 2021, 1.2 million more people were identified as having a disability than were in 2020. Within the portion of that population participating in the labor force, there were 496,000 more people with a disability. As noted in a recent article, “as many as 61 million, or 1 in 4, U.S. adults live with some form of disability, according to the Centers for Disease Control and Prevention. Those numbers are being bolstered by between 7 million and 23 million long-haulers — including 1 million who can no longer work — according to recent government estimates.” Statistics experts, ‘think tanks’ and disability groups expect the numbers to rise as COVID settles in as an endemic disease.
Urgent need for help. The potentially staggering number of affected individuals who may experience the effects of long COVID requires urgent intervention by policy makers and planners right now to anticipate and prepare for the impact of this new cause of disability. This includes addressing the implications for federal and private worker’s compensation and disability insurance programs and support services. Both the federal government and local governments must recognize long COVID as a disability and provide sufferers the same protections as any other disability. According to a recent guidance issued by the Department of Health and Human Services (HHS) under the current administration, long COVID is now recognized as a disability under the Americans with Disabilities Act, Rehabilitation Act of 1973, and the Patient Protection and Affordable Care Act. For a case of long COVID to qualify for long-term disability insurance benefits, you must show that your symptoms substantially limit your ability to perform one or more major life events (such as standing, sitting, or walking), or have caused a mental or physical impairment. This impairment could be anything from lingering mental illness to heart damage, but it must be proven to be linked to long COVID. Long COVID can be helped – with the right protocols and medical advisement. The emergence of long COVID would best be understood as a “mass disabling event” of historic proportions, with the health-care system struggling to absorb an influx of infirmity, and economic growth blunted for years to come. We need Centers of Excellence for treating long COVID including the vaccine injured. Patients must have clinical services to manage long COVID that should be adequately staffed by clinicians that truly understand the complexity of this problem. If addressed early and with the right treatment modalities, many times we can help these patients with full recovery. We are learning more every day. The more we learn, the more HOPE we can offer to the massive numbers suffering from the debilitating impacts of long COVID syndrome. In hope and healing, Dr. Suzanne Gazda References and additional reading: Pomeroy, C. A Tsunami of Disability Is Coming as a Result of ‘Long COVID’. Scientific American. July 6, 2021. https://www.scientificamerican.com/article/a-tsunami-of-disability-is-coming-as-a-result-of-lsquo-long-covid-rsquo/ Danish, J. Long COVID Disability Benefits: 7 Things You Need to Know. Bryant Legal Group. February 22, 2022.https://bryantlg.com/blog/long-covid-disability-benefits-7-things-you-need-to-know/ Bach, K. Is ‘long Covid’ worsening the labor shortage? Brookings. January 11, 2022 https://www.brookings.edu/research/is-long-covid-worsening-the-labor-shortage/ Mazer, B. Long COVID Could Be a ‘Mass Deterioration Event’. The Atlantic. June 15, 2022. https://www.theatlantic.com/health/archive/2022/06/long-covid-chronic-illness-disability/661285/ Wark, P. We need to brace for a tsunami of long COVID. But we’re not quite sure the best way to treat it. The Conversation. June 27, 2022. https://theconversation.com/we-need-to-brace-for-a-tsunami-of-long-covid-but-were-not-quite-sure-the-best-way-to-treat-it-183824 National Institutes of Health https://covid19.nih.gov/news-and-stories/study-looks-risk-factors-long-covid Cleveland Clinic https://consultqd.clevelandclinic.org/obesity-may-increase-risk-of-long-term-covid-19-complications/ Thompson, E., Williams, D. et al. Risk factors for long Covid: Analysis of 10 longitudinal studies looking at HER in the UK preprint 2021. medRxiv. https://www.medrxiv.org/content/10.1101/2021.06.24.21259277v2.full. doi: https://doi.org/10.1101/2021.06.24.21259277 Gazda, S.K. The lingering neurological and other effects of long COVID. (December 2021) https://www.suzannegazdamd.com/blog---long-covid/the-diverse-neurological-and-other-symptoms-of-long-covid Sauerwein, K. Long COVID poses risks to vaccinated people, too. Washington University School of Medicine in St. Louis.May 25, 2022. https://medicine.wustl.edu/news/long-covid-19-poses-risks-to-vaccinated-people-too/ MedAlerts.org https://www.medalerts.org/vaersdb/findfield.php?TABLE=ON&GROUP1=CAT&EVENTS=ON&VAX=COVID19 Zimmermann, Petra MD, PhD, Pittet, Laure F. MD-PhD Curtis, Nigel FRCPCH, PhD. How Common is Long COVID in Children and Adolescents? The Pediatric Infectious Disease Journal. (December 2021) Volume 40 - Issue 12 - p e482-e487 doi: 10.1097/INF.0000000000003328 https://journals.lww.com/pidj/Abstract/2021/12000/How_Common_is_Long_COVID_in_Children_and.20.aspx Cohen K, Ren S, Heath K, Dasmariñas M C, Jubilo K G, Guo Y et al. Risk of persistent and new clinical sequelae among adults aged 65 years and older during the post-acute phase of SARS-CoV-2 infection: retrospective cohort study BMJ2022; 376 :e068414 doi:10.1136/bmj-2021-068414. https://www.bmj.com/content/376/bmj-2021-068414 Davis, N. Two million people in UK living with long Covid, find studies. The Guardian. June 1, 2022. https://www.theguardian.com/world/2022/jun/01/two-million-people-in-uk-living-with-long-covid-say-studies Statista https://www.statista.com/topics/6084/coronavirus-covid-19-in-the-us/#dossierKeyfigures Pan American Health Organization https://www.paho.org/en/news/29-6-2022-covid-19-cases-continue-rise-americas-many-are-risk-developing-post-covid-condition Ziyad, A. Bowe, B., Xie, Z. Outcomes of SARS-CoV-2 Reinfection. Research Square. 17 June 2022. https://www.researchsquare.com/article/rs-1749502/v1 CDC and long-term effects of COVID. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html Center for American Progress https://www.americanprogress.org/article/covid-19-likely-resulted-in-1-2-million-more-disabled-people-by-the-end-of-2021-workplaces-and-policy-will-need-to-adapt/ U.S. Bureau of Labor Statistics https://www.bls.gov/cps/definitions.htm#population https://www.bls.gov/cps/definitions.htm#disability Sellars, F.S. How long covid could change the way we think about disability. Washington Post. June 6, 2022. https://www.washingtonpost.com/health/2022/06/06/long-covid-disability-advocacy/ Guidance on “Long COVID” as a Disability Under the ADA, Section 504, and Section 1557. U.S. Department of Health & Human Services. July 2021. https://www.hhs.gov/civil-rights/for-providers/civil-rights-covid19/guidance-long-covid-disability/index.html McCone, C. We need answers to these four long Covid questions. The Guardian. 30 March 2022. https://www.theguardian.com/world/commentisfree/2022/mar/30/long-covid-coronavirus-covid-pandemic-health Freyer, F. Groups hardest hit by COVID-19 appear least likely to get care for its lingering effects. Boston Globe. March 7, 2022. https://www.bostonglobe.com/2022/03/07/metro/groups-hardest-hit-by-covid-19-appear-least-likely-get-care-its-lingering-effects/
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorSuzanne Gazda M.D. Neurologist Archives
January 2024
Categories |


 RSS Feed
RSS Feed