New data, “old” drug, new hope.
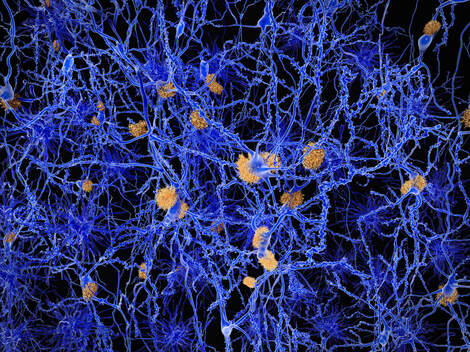
Since scientists first reported that minocycline showed neuroprotective effects in animal models of ischemic injury and that it easily crosses the blood brain-barrier, minocycline has sparked new interest for potential applicability in neurological treatments. Take, for example, this recent article in Brain Behavior and Immunity, “Minocycline prevents the depressive-like behavior through inhibiting the release of HMGB1 from microglia and neurons.” Researchers looked at both minocycline and high mobility group protein box 1 (HMGBI), which is a sophisticated “danger signal” with pleiotropic functions that has been proved to function as a pro-inflammatory cytokine. In the central nervous system (CNS), HMGB1 can stimulate microglia, the immune cell in our CNS, to release inflammatory factors that cause chronic neurodegeneration. It was clearly chronic stress that released HMGBI into these nervous system cells. Think about that – unremitting stress, especially in these times, is really something we have to control if at all possible to give our brains and our immune systems a fighting chance against disease. And if you look at even more of the current data,* it appears that inhibiting the HMGB1/RAGE/TLR4 signaling axis could be a novel therapeutic strategy against several HMGB1 mediated conditions like TBI, neuroinflammation, epilepsy, neurodegenerative diseases and cognitive dysfunction, and, given this latest study, could also improve depressive states. Isn’t the challenge then to identify the means that patients may be able to tolerate a high enough dose where it is actually therapeutic? Perhaps we should consider whether it is possible to create a liposomal version of this drug - this mode of delivery offers a targeted method to get medicines or supplements into the bloodstream without being destroyed by the digestive enzymes or stomach acid and may help alleviate those side effects typically found with higher dose minocycline. Definitely something to think about and news to keep in mind! *Additional reading: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6738663/ HMGB1 involved in stress-induced depression and its neuroinflammatory priming role: a systematic review. https://pubs.acs.org/doi/10.1021/acschemneuro.9b00640 Potential Neuroprotective Effect of the HMGB1 Inhibitor Glycyrrhizin in Neurological Disorders. https://www.frontiersin.org/articles/10.3389/fnins.2018.00628/full HMGB1: A Common Biomarker and Potential Target for TBI, Neuroinflammation, Epilepsy, and Cognitive Dysfunction. _________________________________________ First, I have to say that I truly applaud the researchers behind this very pragmatic study looking at an older drug for treating Alzheimer’s disease (AD). And I'll venture to say too that the cost of this trial was a fraction of what “Big Pharma” has spent on their AD trials that have failed. So often, without a lucrative financial reward behind the trial design, it is extremely difficult to get studies done that employ inexpensive therapies such as minocycline. Minocycline has been studied in multiple neurodegenerative conditions including CVA, MS, Huntington's, ALS, PKD, TBI, and others. In animal models it has been shown to easily cross the blood brain barrier (BBB), be neuroprotective, reduce microglial cell activation, improve mitochondrial function, regulate cell death and reduce amyloid and tau protein. Some believe it works early in the course of disease and or perhaps its positive effects simply wane over time. Others worry about its efficacy due to antimicrobial resistance and gut dysfunction from chronic antibiotic use. The study and its results. The Minocycline in Alzheimer Disease Efficacy (MADE) trial was a double-blind randomized trial, which investigated the administration of 200 mg or 400 mg of minocycline hydrochloride over 24 months in patients with mild AD (avg. MMSE was 26.4); 544 patients were followed for the full two years from 2014 to 2016. The MMSE and the Bristol Activities of Daily Living Scale (BADLS) were used as outcome measures. Some of the key takeaways: 1. Only 29% of the high dose group were able to complete the trial due to SE's and the other groups tolerability weren't much better either (placebo 64% vs 200 mg group 62%). 2. Eligibility criteria were practical requiring 2011 McKhann criteria for possible or probable Alzheimer’s disease, without an upper age limit, MMSE score greater than 23, and, most importantly, that a participant have capacity to provide informed consent. Eligibility was assessed without reliance on extensive neuropsychological testing, volumetric or molecular imaging, or cerebrospinal fluid assays for biomarkers. 2. The slight decrease in the MMSE score over 24 months in the combined minocycline group was similar to that in the placebo group (4.1 vs 4.3 points) and that worsening of BADLS scores over 24 months was also similar in all groups. 3. Minocycline did not delay the progress of cognitive or functional impairment in people with mild AD during a 2-year period. This study also found that 400 mg of minocycline is poorly tolerated in this population. But did it REALLY not work?? Would we see benefit if this treatment was used along with the Bredesen protocol or in conjunction with other outcome measures? Perhaps it should be combined with other things that could enhance mitochondrial function (e.g. CoQ10). Would it work if used in early or preventative strategies (such as a CIS MS trial (clinically isolated syndrome )? Minocycline did seem to help reduce risk of MS progression, but only within the first six months and another trial showed benefit when used along with Copaxone. https://www.nejm.org/doi/full/10.1056/NEJMoa1608889 Other research shows that “animal studies, from which much of the evidence for minocycline as an anti-inflammatory and anti-AD agent come, generally used higher doses of minocycline (typically equivalent to 3-7 g per day in humans. Maybe we shouldn’t be so quick to dismiss the findings in this particular study if it’s possible further review and combination therapies could in fact be useful in helping our patients suffering from milder Alzheimer’s disease. For more information and the full study paper see: https://jamanetwork.com/journals/jamaneurology/fullarticle/801762
1 Comment
Your comment will be posted after it is approved.
Leave a Reply. |
Authorby Suzanne Gazda M.D. Archives
August 2021
Categories |
 RSS Feed
RSS Feed