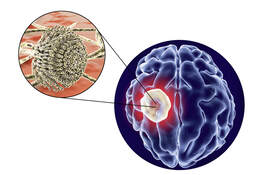
 This recent study showed that patients with multiple sclerosis (MS) have reduced IgG levels, while prior studies also showed a link to other types of autoimmune diseases and similar low IgG levels. We need to ask why this matters and why does this occur? And just as important, what can we do with this new information to positively impact our treatment approaches? Low IgG levels indicate serious immune dysregulation, which could increase a patient’s risk of getting an infection, cancer or autoimmune disease. IgG are immune cells; when your body feels it is under attack, it makes special proteins called immunoglobulins or antibodies. These antibodies are made by B cells and plasma cells and are released throughout the body to help kill bacteria, viruses and other germs.
This particular 2019 study, published in Therapeutic Advances of Neurological Diseases, demonstrated that a substantial proportion of patients with MS had serum IgG concentrations below the lower limit of normal (LLN). Researchers noted that these levels were influenced by the MS disease course and certain immunotherapies (rituximab, intravenous corticosteroids, natalizumab, and fingolimod). So we must ask if whether we are setting up our patients for future serious side effects with some of the disease-modifying therapies that cause further immunosuppression. For example, might we be worsening the immune dysregulation that may have caused the problem in the first place? Certainly, while MS therapies can be beneficial, there is no doubt that some of these treatment options can lead to serious consequences or even death. We know too that all patients with MS have a dysregulated immune system, which is considered to be multifactorial, involving a ‘perfect storm’ of genetic susceptibility, epigenetic and post-genomic events and environmental factors. No one just “walks in the door and gets MS” and if we identify the various potential environmental triggers and carefully address these, perhaps we can remarkably improve a patient's autoimmune disease. The “cross talk” between the innate and adaptive immune system is an ongoing process that may be opening the door for MS as well as continued disease progression. Antigen-presenting cells in the periphery are the spark that begins the cascading levels of immune dysregulation thru the concept of molecular mimicry causing what is essentially “bystander activation.” Given all these potential inciters of disease, I believe that unless we address the root causes of MS, it will continue to be very difficult to effectively treat this neurodegenerative disease. IVIG can indeed be a very beneficial treatment for MS and other autoimmune diseases because of its multiple mechanisms of boosting the immune function. We know that animal models have also shown the potential for IVIG to remyelinate, or help regrow the protective sheath, of our body’s neurons. Now with this study's findings, it is no wonder we are seeing the benefits following IVIG treatment in our MS patients. I look forward to more information being made available that points to similar results and can better guide our approaches and options for our patients’ wellbeing. References: Zoehner G, Miclea A, Salmen A, et al. Reduced serum immunoglobulin G concentrations in multiple sclerosis: prevalence and association with disease-modifying therapy and disease course. Published September 27, 2019, accessed October 28, 2019. https://journals.sagepub.com/doi/full/10.1177/1756286419878340?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub%3Dpubmed. A basic overview of multiple sclerosis immunopathology, European Journal of Neurology 2015, 22 (Suppl. 2): 3–13 Cusick MF, Libbey JE, Fujinami RS. Molecular Mimicry as a Mechanism of Autoimmune Disease. Clinical reviews in allergy & immunology. 2012;42(1):102-111. Chastain, E. M. L. and Miller, S. D. (2012), Molecular mimicry as an inducing trigger for CNS autoimmune demyelinating disease. Immunological Reviews, 245: 227–238. The Enigmatic Role of Viruses in Multiple Sclerosis: Molecular Mimicry or Disturbed Immune Surveillance? Gegenant A ,et al . Trends in Immunology Published: May 23, 2017DOI: https://doi.org/10.1016/j.it.2017.04.006 Immunoglobulins stimulate cultured Schwann cell maturation and promote their potential to induce axonal outgrowth . Nevena Tzekova, André Heinen, et al. Journal Of Inflammation May 2015 https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-015-0331-
1 Comment
Your comment will be posted after it is approved.
Leave a Reply. |
Authorby Suzanne Gazda M.D. Archives
August 2021
Categories |
 RSS Feed
RSS Feed